Introduction
An alveolar bone exostosis is a rare but notable complication that can arise during or after orthodontic treatment. Exostosis refers to the formation of a benign bony outgrowth on the surface of bones. These bony growths are typically non-malignant and can vary in size and shape depending on factors such as mechanical stress, inflammation, and genetic predisposition (MacDonald-Jankowski, 2012).1
Clinically, patients with this condition may present with noticeable bony swellings on the buccal(cheek), labial side of the maxilla. These swellings are often asymptomatic but can cause discomfort, tenderness, or irritation in some cases. Additionally, the presence of these bony outgrowths can complicate oral hygiene practices and affect the overall aesthetics of the smile.
Radiographic examination and clinical evaluation are essential for an accurate diagnosis of buccal exostosis. Differential diagnosis is most significant to decide exostosis from other pathologic conditions like fibrous dysplasia, osteomas, and other bony lesions. Cone-beam computed tomography (CBCT) and panoramic radiographs are commonly used imaging modalities that provide detailed visualization of the bony outgrowths and their relationship to surrounding structures.
The etiology of orthodontically induced buccal exostosis is multifactorial. Factors such as excessive orthodontic forces, prolonged treatment duration, and individual biological response to mechanical stress play significant roles in the development of these bony protuberances. Genetic factors may also contribute, as individuals with a familial history of exostosis or other bony anomalies may be more predisposed to developing such conditions.
Etiology of exostosis during orthodontic treatment 2
Exostosis, or bony outgrowths, can develop during orthodontic treatment due to several aspects:
Genetic predisposition
Genetic aspect play a important role in the progress of exostoses. Hereditary multiple exostoses (HME) is an autosomal dominant disorder characterized by multiple osteochondromas, caused by mutations in the EXT1 or EXT2 genes.
Mechanical stress
The continuous mechanical forces exerted by orthodontic appliances on teeth and surrounding bone structures can stimulate the periosteum, leading to the formation of exostoses. This is particularly evident in areas subjected to high stress during tooth movement.
Environmental factors
Chronic irritation or inflammation of the periosteum due to orthodontic appliances can also contribute to the development of exostoses. This is often seen in areas where the appliances exert pressure.
Functional influences
Functional habits such as bruxism (teeth grinding) or clenching can exacerbate the formation of exostoses by increasing mechanical stress on the bone.
Nutritional factors
Nutritional factors, including higher units of polyunsaturated fatty acids or vitamin D, have been suggested as potential contributors to the development of exostoses.
Understanding these etiological factors is crucial for diagnosing and managing exostoses during orthodontic treatment. Proper identification and management can help mitigate potential complications and ensure successful orthodontic outcomes.
Management of orthodontically induced buccal exostosis involves a comprehensive approach tailored to the severity of the condition and the patient's symptoms. In mild cases, conservative management with regular monitoring may be sufficient. However, in more severe cases where the exostosis causes significant discomfort, functional impairment, or aesthetic concerns, surgical intervention may be required to remove the bony outgrowths. Treatment choices vary from conservative monitoring to surgical intervention, depending on the severity of exostosis and the patient's symptoms.
This present case report explains the surgical management of orthodontically induced alveolar buccal bone exostosis.
Case Presentation
A 20-year-old female patient was undergoing orthodontic treatment in Department of Orthodontics and Dentofacial Orthopedics of S.B. Patil dental college and research, Bidar. Post alignment and leveling, during the retraction phase, bilateral masses from the right premolar to the left premolar area in the maxilla interfering with her smile and aesthetics, as well as prohibited retraction. On clinical examination, large bilateral overgrowths were situated on the buccal and labial aspect of the maxilla between the right to left premolar region, involving the marginal and attached gingiva. The bony prominences were firm and ovoid in shape, with the gingiva above them appearing pale and thin. A final diagnosis of alveolar buccal bone exostosis was done after CBCT evaluation and blood investigation. Pre-treatment and during orthodontic treatment intraoral photographs are given in (Figure 1, Figure 2).
Orthodontic treatment
Extraction of 1st premolars in 1st, 2nd and 3rd quadrant was done as case was diagnosed as Angle’s class II division I subdivision malocclusion with convex soft tissue profile, followed with individual canine retraction as en mass retraction might be delayed because of ABE(ALVEOLAR BONE EXOSTOSIS) and exacerbate the bony lesion due to higher orthodontic force used for en mass retraction. After alignment and leveling, the individual canine retraction was done followed by Final space closure with loop mechanics (Teardrop loop) was planned.
Pre surgicalprocedure
Oral prophylaxis and root planning was done as phase I therapy. Patient was recalled after 1 week and accessed. After evaluation resective osseous surgery was planned for removal of alveolar buccal bone exostosis. After obtaining the permission from institutional ethical committee, informed consent was taken from the patient.
Surgical procedure
Local anesthesia was administered (1:80000 epinephrine). Sulcular incision was done from right first premolar to left first premolar. Vertical releasing incision was given wherever it was necessary. A full-thickness mucoperiosteal flap was then reflected using the periosteal elevator for observing nodular osseous area.
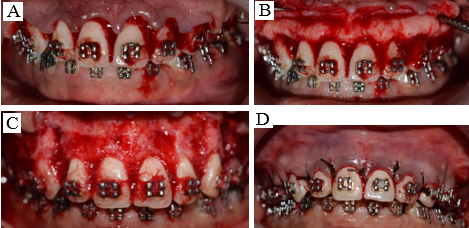
Resective osseous surgery was performed with the following steps using carbide burs. Vertical grooving, radicular blending, flattening of the interproximal area & gradualising the marginal bone. Micro perforations were done bilaterally mesial to the canine for accelerated orthodontic movement. After cleaning the area with normal saline solution, a flap was closed with 3-0 silk sutures. Intraoral photographs during the surgical procedures are given in (Figure 3A,B,C,D).
Outcome and follow-up
Postoperative instructions and oral hygiene instructions were given to the patient. Antibiotics, analgesics, and a 0.2% chlorhexidine gluconate mouth rinse were prescribed. Next 7 days, the patient was assessed for any uneventful postoperative discomfort and healing. Oral hygiene instructions were reinforced, and a supportive periodontal therapy session was planned after a month. One-month later, active orthodontic therapy was resumed. Intraoral photographs at 3 weeks, 3 months and 6 months are given in (Figure 4, Figure 5, Figure 6).
As we can see in (Figure 6) that after six months of surgical removal of ABE there is some rebound of ABE in the premolar-to-premolar region, which is expected to cease once the orthodontic treatment is completed. 2
Discussion
Buccal exostosis is a benign, slow-rising bony protuberances on buccal alveolar bone that has been considered to be a common indication for osseous resection during periodontal surgery. 3, 4 Though an exostosis typically requires no treatment, it can be resected with minor osseous surgery to bring back the patient’s gingival architecture, lessen lip strain, control food retention over the bone, and decrease traumatic ulceration during oral hygiene. 5
Glickman and Smulow, when new bone formation is observed on the external surfaces of the alveolar ridge adjacent to traumatized teeth, it indicates that buttress bone formation is occurring. This process serves to strengthen the trabecular bone as a functional adaptation. 6
Our case report demonstrates the growth of alveolar bone exostoses that prominently developed during alignment and after start of retraction of upper anterior teeth. Several factors can influence changes in alveolar bone thickness during the retraction of incisors. These include the speed of tooth movement, the degree of buccolingual tilt, and the extent of the upper incisor intrusion, and use of orthodontic implants
Although the exact mechanism behind the progress of alveolar bone exostoses following orthodontic treatment remains unclear, some evidence suggests a connection to the thickening of the labial aspect of the alveolar bone due to the hasty retraction of the upper incisors.7 The damage brought on by orthodontic forces, which results in the release of bone morphogenic proteins, which are expressed as exostoses and ossify at the stress points, may be the origin of the formation of buttressing bone. Rapidly retracted anterior teeth cause cortical bone remodelling to stall because it cannot keep up with the movement.8 It is a well-known fact that cortical bone remodelling is dependent on the direction of tooth movement in the horizontal, vertical, and sagittal planes. 9
Yodthong et al. investigated how the thickness of their alveolar bone varied in response to the degree of intrusion, angulation, inclination, and rate of tooth movement. According to the study, when the incisors were retracted, the alveolar bone's thickness increased.10
The 2006 study by Tang et al. showed that mechanical straining can produce morphological alteration and a magnitude-dependent increase in the expression of bone morphogenic protein-2, alkaline phosphatase, and collagen type I mRNA in osteoblast-like cells, which may affect bone remodelling during orthodontic treatment. 11
Future studies to be conducted to determine the correlation between the amount of force, direction of force and type of force (intermittent, continuous) used while orthodontic treatment in subjects with alveolar bone exostosis formation
Conclusion
This case report shows that there is enlargement of alveolar bone exostoses following the retraction of upper anterior teeth. Multifactorial influence changes the alveolar bone thickness during incisor retraction, such as the rate of orthodontic tooth movement, the degree of buccolingual tilt, and the extent of upper incisor intrusion, and also the use of orthodontic implants in some cases. Furthermore, we have successfully demonstrated surgical methods to eliminate ABE during orthodontic treatment and complete cessation of ABE is expected after completion of orthodontic therapy. As available research have not mentioned about exact corelation between the rate of retraction during orthodontic tooth movement and ABE, future studies need to be done.