Introduction
Saliva is important in the maintenance of oral health by exhibiting numerous host defense functions such as lubrication, anti-microbial activity, control of mineralization potential of teeth and others.1 The unstimulated salivary flow rate is 0.1-0.3ml/min, with an average total of 16 hours of unstimulated saliva flow being 300 ml with a pH 7.2 -7.4.2 Salivary flow rate during sleep is nearly zero. The maximum stimulated salivary flow rate is 1.5-7ml/min. 80-90% of the daily salivary secretion is produced by stimulated saliva. 3
This miraculous fluid of oral cavity also reflects the systemic condition of an individual. Hypo-salivation is seen in patients with renal problems, hypertension, and diabetes. Significant changes in salivary output and its composition are also seen in anxiety, depression disorders, stress and other systemic diseases.4 Hypertension is a highly prevalent cardiovascular disease, which affects over 1 billion people worldwide. Although more than 70% of hypertensive patients are aware of the disease, only 23.49% are treated, and fewer (20%) achieve control. Hypertension is defined as systolic and diastolic blood pressures with values >140mmHg and >90mmHg respectively, the prevalence of which varies by age, race, and education.4 In 2017, new guidelines from the American Heart Association, the American College of Cardiology, and nine other health organizations lowered the numbers for the diagnosis hypertension to 130/80 millimetres of mercury (mm Hg) and higher for all adults. The previous guidelines set the threshold at 140/90 mm Hg for people younger than age 65 and 150/80 mm Hg for those ages 65 and older as shown in (Table 1).5 Saliva is gaining popularity as a diagnostic tool for evaluating physiologic and pathologic conditions by virtue of its ease of collection method, non-invasiveness and low cost.6, 7 Thus, the aim of the present study was to evaluate the influence of controlled and uncontrolled hypertension on pH of saliva and saliva flow rate.
Table 1
Blood pressure categories. 5
Materials and Methods
This study included 60 patients of age between 20 to 60 years, who came with various health problems to the department of General Medicine of Mahavir hospital, Vikharbad, Telangana, India.
Inclusion criteria
Patients aged between 20 and 60, with stage 1 hypertension while on medication, with stage 2 hypertension even after consuming medication, and patients with no hypertension who were willing to participate in the study were taken as the control group.
Exclusion criteria
Patients with systemic diseases and on medications for the same were excluded. Specific diseases that affect the salivary output/composition like diabetes mellitus, Sjogren’s syndrome, malignancies and its complications were also excluded.
Patients were selected randomly then signature on consent form was taken and a proper case history was recorded after which they were divided into three groups:
Group A - 30 individuals without hypertension and do not use any medication
Group B – 30 individuals with Stage 1 hypertension (130 – 139 by 80 - 89) even after consumption of medication
Group C – 30 individuals with Stage 2 hypertension (140 or higher by 90 or higher) even after consumption of medication.
The stages given by American heart association in 2017 were considered.
From each patient saliva was collected in a sterile Polypropylene Centrifuge Tube. Five minutes later, the flow rate was monitored and the lid was fastened. For pH, pH strips were used and pH was estimated with the help of pH stencil provided by the pH strip company.
After checking the flow rate and pH of the saliva the values were noted in their particular groups and sent for statistical analysis.
Results
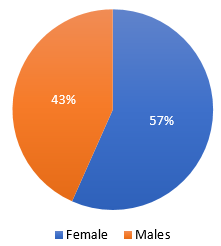
In the present study, the subjects were selected by random sampling method in which 57% were female and 43% were male. (Figure 1)
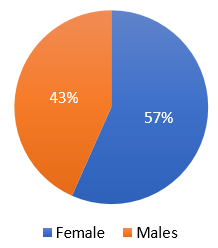
In the present study, the subjects were selected by random sampling method in which 57% were female and 43% were male. (Figure 2)
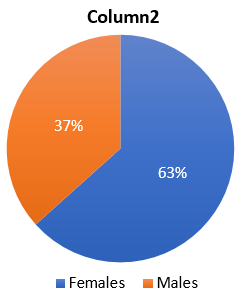
In the present study, the subjects were selected by random sampling method in which 63% were female and 37% were male. (Figure 3)
Mean and standard deviation of salivary pH in 3 groups.Table 2
Table 2
Mean and standard deviation of salivary pH in 3 groups
|
Groups |
Std. Deviation |
Mean |
Number |
|
Group 1 |
0.43628 |
6.487 |
30 |
|
Group 2 |
0.50526 |
6.060 |
30 |
|
Group 3 |
0.56959 |
5.851 |
30 |
|
ANOVA TEST p= 0.000 |
|||
Multiple comparison of salivary pH in 3 groups.Table 3
Table 3
Multiple comparison of salivary pH in 3 groups
Mean and Standard deviation of saliva displacement in sterile polypropylene centrifuge tube (mm/10s) amongst 3 groups.Table 4
Table 4
Mean and Standard deviation of saliva displacement in sterile polypropylene centrifuge tube (mm/10s) amongst 3 groups
|
Groups |
Std. Deviation |
Mean |
Number |
|
Group 1 |
2.6310 |
4.678 |
30 |
|
Group 2 |
1.9932 |
3.233 |
30 |
|
Group 3 |
1.6963 |
2.556 |
30 |
|
ANOVA TEST p= 0.000 |
|||
Multiple comparisons of the saliva displacement in Polypropylene Centrifuge Tube amongst 3 groups.Table 5
Table 5
Multiple comparisons of the saliva displacement in Polypropylene Centrifuge Tube amongst 3 groups
Discussion
The results of this study demonstrated the relationship between hypertension, antihypertensive medications, and their influence on saliva properties. The participants involved in this study were only hypertensive individuals without any other systemic diseases and a few of them took particular medications for their high BP (such as losartan, beta -blockers) but not diuretics because it has been shown that diuretics cause xerostomia. 8, 9
To remove the differences among examiners, an automatic sphygmomanometer was employed. Unfortunately, a few studies have been done on the effects of hypertension on saliva. In a study, R. Kagawa et al.8 found that pH of unstimulated saliva is significantly lower in hypertensive individuals. In fact, their results showed that the increase in both systolic and diastolic BPs could lead to decrease in pH of unstimulated saliva.8 The results of current study showed that the decrease in saliva pH and hypertension are related; this finding is similar to R. Kagawa’s8 results. Our results showed that pH of unstimulated saliva in stage I hypertensive individuals (Table 2) and borderline participants was lower than those with normal BP, therefore, a reduction in pH can cause changes in physical and chemical properties of saliva , which subsequently may influence the oral health. 10, 11
Preoteasa et al. 12 expressed that viscosity and pH of saliva are both independent parameters and their changes are not related to each other; while pH decreases, viscosity tends to increase. This is consistent with our results, as we also did not find any relationship between saliva viscosity and pH in the participants in our study.
The viscosity of samples was measured just immediately after collection due to the possibility of its rapid changes by time. As mentioned in previous studies, temperature can negatively influence the viscosity of saliva; therefore, in the current study the amount of sample displacements in sterile polypropylene centrifuge tube was measured at 25°C to prevent the effect of temperature.13 The statistical analysis of this study showed that, the amount of salivary displacement in the thistle tube in stage I and pre hypertensive groups was significantly lower than normotensive group. Therefore, the viscosity value was higher in hypertensive groups and because of higher viscosity, saliva travels less in the sterile polypropylene centrifuge tube in the hypertensive groups (Table 4). It can be inferred that by increasing BP, the viscosity of unstimulated saliva also increases resulting in lower salivary flow (Table 5).This would consequently influence the cleansing effect of saliva on teeth and oral mucosa resulting in impaired oral health in these individuals. 14
In addition, pH of samples was measured immediately after collection because pH of saliva increases while it is exposed to the air due to constant losing of CO2.15 The findings of current study showed that pH of unstimulated saliva in stage I hypertensive and pre-hypertensive groups was significantly lower than in normotensive group. It may be suggested that the decreased salivary pH in patients with hypertension could be related to the reduction of unstimulated salivary flow
rate in these patients before taking medications. This might be due to higher activity in the sympathetic pathways and lower activity in the parasympathetic pathways, which controls the salivary secretion and leads to lower salivary flow rate.16 Moreover, bicarbonate (the most important oral buffer) is more effective in higher salivary flow rates and in lower flow rates its concentration decreases extremely, resulting in lower pH, (Table 3) and buffering capacity of the saliva. 17 It could be stated that, pH of saliva is dependent on the amount of secreted saliva and the speed which is secreted by the salivary glands, therefore, influencing the components of the saliva. Besides, because of decreased saliva secretion in high BP patients, pH is reduced and buffering capacity is compromised.18, 19, 20 The reason for this increase in bicarbonate concentration is the elevation of saliva secretion rate, and in general, bicarbonate concentration is low in all salivary glands. However, when metabolic activity is increased, CO2 is produced and is hydrated by carbonic anhydrase enzyme, therefore, lower saliva secretion results in lower bicarbonate concentrations. 21 Salivary buffering capacity has a great influence on pH of plaque surrounding the enamel and plays an important role in prevention of dental caries progression.22 Therefore, in individuals with high BP, the concentration of bicarbonate and consequently its buffering capacity diminishes because salivary flow rate and saliva pH is reduced in these patients. If this reduced pH in oral cavity is sustained for a long period, it can lead to colonization of non- useful bacteria, which leads to higher caries rate compared to normotensive individuals and the oral health of the patient is compromised.23 It is reported that salivary viscosity is related to salivary protein content,24 therefore, any alterations in protein secretion of saliva modifies its properties and these changes lead to irreversible complications in oral health.25 Lubrication of mouth, larynx, and other soft and hard tissues is one of the most important roles of saliva, which is made by elastic resistance between surfaces, and viscosity is the most important indicator of saliva lubricating role.26 Consequently, increased viscosity results in rampant caries, oral mucositis, difficulty in swallowing, halitosis, and the early tooth loss due to caries, which all these consequences may influence the life quality of a patient with hypertension. 27, 28, 29 It seems reasonable to monitor chronic hypertensive patients that take antihypertensive medications and have a history of root caries or periodontal diseases more frequently. 30
In this study, one of our limitations was the small sample size of patients who were taking medication in stage I hypertension; therefore, we could not compare subjects taking medication with those who did not. However, for reducing the effect of medication, patients taking medications with known effects on BP were excluded from the study. Future studies are suggested to be done only on patients with stage II hypertension who are taking the same medication for better results.