Introduction
Alveolar osteogenic orthodontics (AOO), or "Periodontally Accelerated Osteogenic Orthodontics" (PAOO), represents a methodical probe aimed at refining orthodontic treatment.1 The surge in orthodontic treatment for non-growing patients, driven by heightened awareness and aesthetic aspirations, prompts a critical examination of associated challenges. These include protracted treatment periods, concerns over dentofacial aesthetics, and the impact of appliance types in use. Notably, the desire for expedited brace removal and reduced treatment duration is underscored.2
Prolonged orthodontic treatment, particularly in adults, is implicated in potential risks such as periodontal disease and consequential bone loss, exacerbating the likelihood of relapse. The consequences range across various conditions characterized by bone and tissue loss, and permanent orthodontic treatment is linked to enamel decalcification, a well-researched issue. In search of the "ideal force" that would cause alveolar bone to respond in the "optimal" way, periodontal and orthodontic and dentofacial orthopaedics specialties have come together to form surgical dentofacial orthopaedics.3
PAOO, as an innovative approach, deviates from the reliance on pre-existing alveolar volume. Noteworthy is its capacity to facilitate tooth movement 2 to 3 times further within a condensed timeframe compared to conventional orthodontic therapy. Furthermore, it has demonstrated potential in circumventing the necessity for certain orthognathic surgeries, offering a minimally morbid treatment modality across a broad age spectrum.3
This article endeavours to provide an extensive analysis of historical overview, biomechanical principles, surgical procedures, indications, clinical applications, contraindications, limitations, complications, and advantages associated with PAOO, thereby contributing to a nuanced understanding of this evolving orthodontic paradigm.
History
The evolution of orthodontic tooth movement with surgical assistance traces its roots to the 1800s, culminating in the modern understanding and innovative techniques we have today. L.C. Bryan's exploration in 1893 laid the foundation for corticotomy-facilitated tooth movement, but it wasn't until 1959 that Kole revolutionized the field with a method for rapid tooth movement.4, 5
Kole's technique involved an invasive approach, with full-thickness flap reflection exposing lingual and buccal alveolar bone. Kole's corticotomy technique was characterized by subapical horizontal cuts and interdental cuts through cortical and medullary bone. However, due to its invasiveness, Kole's technique faced limited acceptance.5
Düker's studies on beagle dogs in the 1960s further validated corticotomy's impact on tooth vitality and the periodontium. It was determined that the periodontium's health was maintained by circumventing the marginal crest bone while performing corticotomy cuts. This was considered in later procedures; whereby interdental cuts were positioned carefully to avoid the alveolar crestal bone.6
In the 1990s, Wilcko et al. introduced Accelerated Osteogenic Orthodontics (AOO), later known as Periodontally Accelerated Osteogenic Orthodontics (PAOO).7, 8 This innovative approach combined corticotomy surgery with alveolar grafting, showcasing safety, predictability, reduced root resorption, and shortened treatment times. This procedure was developed in 1995 by the Wilcko brothers, Dr. William and Dr. Thomas Wilcko, who specialize in orthodontics and periodontia, respectively. They combined corticotomy with their research on the "Regional Acceleratory Phenomenon" (RAP), which was first described by Harold M. Frost in 1980.9
In contrast to osteotomy, which cuts through both of cortical and medullary bone, corticotomy is characterized as a surgical operation that exclusively modifies the cortical bone. Heinrich Kole's emphasis on disrupting the dense cortical bone layer, known as "bony block movement," influenced the field.5 However, Wilcko et al.'s 2001 publication challenged this concept, revealing that a temporary demineralization/remineralization procedure in the alveolar housing caused the rapid movement of teeth, which was consistent with the RAP healing pattern.7
To enhance bony volumes post-orthodontic forces, the Wilcko brothers combined corticotomy-facilitated orthodontics with alveolar augmentation to create a more refined method. This comprehensive approach became known as the Accelerated Osteogenic Orthodontics (AOO) technique and, now known as the PAOO surgical technique.8, 9 These advancements contribute significantly to the evolving landscape of surgical orthodontic therapies, providing safer, more predictable, and efficient alternatives to traditional orthodontic treatments.
Biomechanics
Frost's seminal work in 1983 established the foundational understanding of Regional Acceleratory Phenomenon (RAP), although histomorphometries had been familiar with the phenomenon since 1966. Frost emphasized that RAP is not a stand-alone healing occasion but rather expedites Hard and soft tissue rehabilitation phases ranging from two to ten times. 9
Recognizing the transformative effects of surgical wounding on osseous tissue, Frost coined the term "The Regional Acceleratory Phenomenon" (RAP), encapsulating a cascade of physiologic healing process. This phenomenon denotes a reaction of local tissues to harmful stimuli, resulting in a local remodelling procedure that accelerates tissue regeneration, with the magnitude of the response directly influenced by the stimulus. Remarkably, compared with conventional bone turnover, RAP promotes bone healing at a rate 10–50 times faster.10
The complex stages of RAP have been thoroughly investigated, especially in the tibia of rat. Initial stages involve the genesis of woven bone, stretching from the surface of bone to the medullary bone, and by day seven, it has reached its maximum thickness. The core of the cortical bridge is formed by this woven bone, crucial for providing mechanical stability after injury. Subsequently, in the medullary area, woven bone experiences temporary resorption, leading to decrease in local bone mineral density, while woven bone in the cortical area remodels to lamellar bone. This phenomenon emphasizes the necessity of medullary bone reconstruction and reorganization following the establishment of a new cortical bone structure in order to accommodate the restoration of cortical integrity. In rat models, this process is especially clear within three weeks.
An additional layer to RAP is provided by the systemic acceleratory phenomenon (SAP), which suggests that humoral factors are released systemically, leading to osteogenesis. Within days of a surgical injury to the human long bones, RAP begins, usually peaking at 1-2 months, and it might take up to 24 months for it to go away entirely. In healthy tissues, this leads to decreased local bone densities (osteopenia) while the volume of the bone matrix stays unchanged. Notably, mild RAP activity can be stimulated by orthodontic force on their own. Nonetheless, the combined action of selective decortication and orthodontic force optimizes the benefits of RAP.10
Notable contributions from Norrdin and Shih showed that temporary bursts of hard- and soft-tissue remodelling occur when intraoral cortical bone injury via corticotomy accelerates normal regional healing processes.11
Wilcko et al. made a significant advancement in 2001 when they modified the original bony block movement technique. They made a trial to conjecture that the patterns of physiologic movement of teeth following decortication of specific area may be related to a demineralization- and remineralization process rather than bony block movement, especially in cases of severely crowded dental arches.7 The Periodontally Accelerated Osteogenic Orthodontics (PAOO) technique was made possible by this realization. In this case, the labial and lingual surfaces of the teeth which has to be translocated undergo surgical scarring of the cortical bone, which is followed by grafting. Recent research indicates that a localized osteoporosis state may be a component of the healing process (RAP) that causes the accelerated tooth movement following PAOO. This fast tooth movement through PAOO is significantly dissimilar from periodontal ligament cell-mediated tooth movement.
Reduced local bone thickness and increase in rate of replacement of new bone from old —which is thought to promote orthodontic tooth movement—are important aspects of RAP in bone healing. Inducing an osteoporosis state, as evidenced by Goldie and King through depleted calcium intake in lactating rats, resulted in increased orthodontic tooth movement, along with reduced root resorption.12 Wilcko et al. provided additional support for these results by presenting radiographic proof of osteoporosis in corticotomy-treated alveolar bone, showing similar acceleration of tooth movement combined with corticotomy cuts and small, round cortical perforations in a split-mouth configuration.
The timeline of RAP's manifestation is critical to understanding its impact on orthodontic interventions. RAP appears soon after the injury, usually peaks between first and second month, lasts for four months in bone, and may take up to twenty-four months to go away. RAP endures as long as movement in the teeth is present. Osteopenia vanishes and radiographic picture of a normal spongiosa resurfaces as RAP goes away. Upon completion of orthodontic tooth movement, an environment is created that favours alveolar remineralization.9
Surgical Procedure 1, 2, 13, 14
Extensive research has focused on the process of altering the equilibrium between resorption and opposition in order to accelerate tooth movement without permanently harming the periodontium. The breakdown-causing osteoclast-mediated activity is essential for controlling the pace of movement of teeth, especially when combined with the periodontal ligament. Orthodontics using corticotomies, also known as corticotomy-assisted or corticotomy-facilitated orthodontics, is gaining popularity as a curative technique which uses carefully planned surgical damage to speed up bone metabolism and promote orthodontic movement of teeth. This treatment, which is positioned as a middle ground between orthognathic surgery and traditional orthodontics, aims to accelerate bone remodelling.
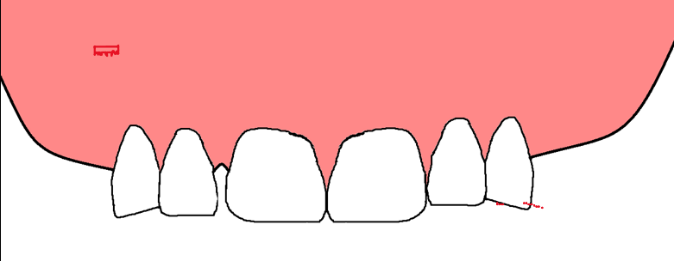
Flap design: (Figure 1)
The flap design serves multiple objectives: providing access to alveolar bone for corticotomies, covering particulate grafts, maintaining interdental tissue height and volume, and enhancing aesthetics. Flap is designed having split-thickness section in the apical regions and complete-thickness flap in its coronal aspect. This split-thickness dissection offers flap mobility for minimal tension suturing. The identification of important neurovascular structures is facilitated by the careful elevation of the periosteal layer, which exposes the alveolar bone. A good esthetic result requires conservation of the interdental gingival tissues, which can be accomplished using a variety of methods for preservation of papillae.
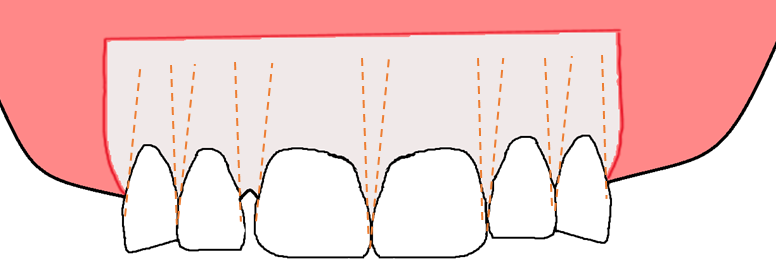
Decortication: (Figure 2)
Decortication aims to initiate the Regional Acceleratory Phenomenon (RAP) response without creating movable bone segments. Utilizing a round burr No. 1 or No. 2 or piezoelectric knife corticotomies are made in alveolar bone, with no specific pattern, depth, or extent superiorly validated. Corticotomies are placed on both lingual and labial aspects, involving vertical grooves in the interradicular space and circular-shaped corticotomies. The procedure avoids extending cuts near neurovascular structures, ensuring safety.
Particulate grafting
Grafting, performed in corticotomy areas, involves products such as deproteinized bovine bone, decalcified freeze-dried bone allograft or autogenous bone. Graft volume is dictated by predicted tooth movement, pretreatment bone thickness, and the demand for labial support. The graft material is cautiously placed, and the decorticated bone acts to retain it. Techniques using platelet-rich plasma or calcium sulphate may enhance graft stability.
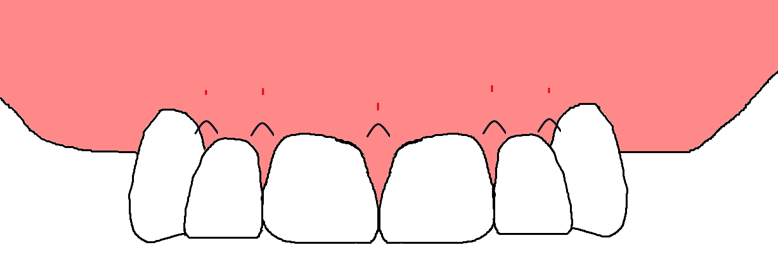
Closure techniques: (Figure 3)
Non-resorbable interrupted sutures are placed to proximate gingival flaps initially while avoiding undue tension and graft containment. Sutures remain in place for 1 to 2 weeks, contributing to therapeutic endpoints.
Patient management
The multiple-hour PAOO surgical procedure requires sedation of the patient. Antibiotics and painkillers are given based on the clinician's preference, while short-term steroids improve the comfort of patients and clinical recovery. Nonsteroidal anti-inflammatory drugs should not be used after surgery as they may disrupt the local acceleratory process. Icepack application is suggested to minimize postoperative swelling or oedema. Common complications include self-limiting oedema and ecchymosis, with postoperative evaluations scheduled every week in first month and then monthly afterwards.
Orthodontic treatment timing
Orthodontic brackets are bonded and then arch wires are activated a week before PAOO surgery. Immediate application of heavy orthodontic force follows flap repositioning, ensuring optimal utilization of the limited RAP window (4-6 months). The orthodontist's strategic approach involves rapidly advancing arch wire sizes to capitalize on the accelerated tooth movement period before transitioning to finishing movements at a normal speed.
Figure 3
Suture placement 1 Non-resorbable interrupted sutures are placed to proximate gingival flaps.
Indications and Clinical Applications
Resolving crowding and reducing treatment duration
PAOO is recommended for cases where dental crowding needs resolution, offering a significant reduction in the overall treatment duration. This application is particularly beneficial for patients seeking expedited orthodontic outcomes. 7
Expediting canine retraction after premolar extraction
The procedure proves advantageous in accelerating the retraction of canines following premolar extraction. By doing so, it enhances the efficiency and effectiveness of orthodontic interventions. 15
Improving post-orthodontic stability
PAOO is indicated to enhance the stability of orthodontic results post-treatment, providing a solution for prolonged positive outcomes. 16
Facilitating eruption of impacted teeth
In cases where teeth are impacted, PAOO is a valuable method to facilitate their eruption. This application addresses challenges encountered in traditional orthodontic approaches for impacted teeth. 14
Enabling slow orthodontic expansion
For situations requiring slow orthodontic expansion, PAOO offers a suitable solution. It ensures a well-regulated and efficient expansion process. 17
Addressing molar intrusion and correcting open bites
PAOO is indicated for molar intrusion, catering to prosthodontic needs, and correcting open bites. This application showcases the versatility of the procedure in addressing various orthodontic challenges. 18
Effective manipulation of anchorage
The procedure is recommended for manipulating anchorage effectively. This application is crucial for achieving optimal orthodontic outcomes, especially in cases where precise control over tooth movement is essential. 19
Contraindications and Limitations 16
Current periodontal disease or recession
Patients suffering from any kind of periodontal disorder or having significant recession in the level of gingiva are not suitable subjects.
Complications and Side Effects
Harmful effects to the periodontium
Reports exist on various adverse effects, from without any complication to decrease in interdental bone, reduction in level of attached gingiva, and observed periodontal deformities in patients with less interdental space. 20
Hematomas in subcutaneous region and post-operative swelling
Intensive corticotomies may lead to hypodermic hematomas of the neck and face, along with expected swelling and pain after surgery for several days. 21
Pulp vitality
No unfavourable consequence on the vitality of pulp in the corticotomy region have been observed. Investigation is needed to evaluate the effect of fast movement on pulp vitality in a longer duration. 22
Root resorption
While little amount of resorption of root is anticipated with any orthodontic movement, the decrease in treatment duration of PAOO may minimize the risk. Studies report safe tooth movement with no associated root resorption in specific cases. 23
Advantages of Corticotomy 5
Prevents periodontal injury and pocket formation
Corticotomy prevents injury to the periodontium and pocket formation, ensuring a more conservative approach compared to osteotomy.
Avoids tooth devitalization
Unlike some other procedures, corticotomy avoids tooth devitalization, preserving pulp vitality during orthodontic treatment.
Shortens treatment time
PAOO significantly shortens the overall treatment time, providing a more time-efficient alternative to conventional orthodontic methods.
Maintains bone nutritive function
The procedure maintains the regular nutritive needs of the bone via spongiosa, even when exposed thus, reducing the chances of bone aseptic necrosis.
Note: It is crucial to assess each patient individually, considering their specific oral health condition and treatment needs, to determine the suitability of PAOO and to manage potential complications effectively.
Conclusion
In conclusion, the Periodontally Accelerated Osteogenic Orthodontics (PAOO) technique transcends traditional tooth alignment, venturing into the realm of facial aesthetics and serving as a tangible manifestation of in vivo tissue engineering. By seamlessly integrating in-office periodontal surgery with orthodontic interventions, PAOO extends its transformative impact beyond isolated dental concerns to encompass the entire lower face's esthetic harmony. Although mastery of modified diagnostic and treatment parameters is requisite, once achieved, orthodontists gain access to a potent treatment avenue for their patients. As the adult demographic increasingly embraces orthodontic solutions, especially considering the susceptibility of adults and some non-growing adolescents to periodontal issues, PAOO emerges as an appealing "win-win" proposition for orthodontists, periodontists, and patients alike.
It substantiates the viability of adult orthodontics. This evolution is indebted to the Regional Acceleratory Phenomenon inducing transient osteopenia, strategically harnessed for addressing diverse clinical complexities such as decrowding and molar intrusion.