- Visibility 891 Views
- Downloads 46 Downloads
- DOI 10.18231/j.idjsr.2024.024
-
CrossMark
- Citation
Evolving interfaces: A comprehensive review of implant-abutment connections
- Author Details:
-
Nikita Narendra Valvi *
-
Smita Khalikar
-
Kishor Mahale
-
Vilas Rajguru
-
Sonali Mahajan
-
Ulhas Tandale
Introduction
Dental implants have been widely accepted as a predictable and reliable tool for dental restoration, but it is still necessary to ensure that the height of the peri-implant crestal bone is maintained (Buser et al., 2002). Albrektsson et al. (1986) proposed that a dental implant can be considered successful if peri-implant crestal bone loss is less than 1.5 mm during the first year after implant placement and less than 0.2 mm annually thereafter.[1], [2]
Since the introduction of dental implants many changes were made in the implant systems to incorporate additional features or modifications to the existing. One among such modifications is design of the connection that allows the prosthetic supra-structure to be attached to the implants.[3], [4]
Clinical research in oral implantology has led to advancements in the biomechanical aspects of implants, implant surface features and implant componentry thus widening the applications of implant dentistry from restoration of a single tooth to multiple missing teeth with predictable success. A dental implant abutment is formally defined as ―that portion of a dental implant that serves to support and/or retain a prosthesis.
Crest module is that portion of implant fixture that provides connection to abutment and consists of a platform & anti rotation features.[5] The success of implant not only depends on osseointegration but also on prosthetic elements. Particularly, the connection between implant and abutment is a key junction because it is the primary determinant of long term stability and strength of implants which in turn determines the final outcome of implant therapy. The implant abutment interface ensures optimal load distribution along with lateral and anti-rotational stability.
Earlier the Branemark system was characterized by an external hexagon which was developed to facilitate implant insertion rather than to provide clinicians with an anti-rotational device. This external hexagon configuration has performed well over the years. But over a period of time the drawbacks of external connection came into light which led to the modification in implant abutment connection.[6]
Search strategy
Search strategy included PUBMED and google scholar from 2000 to 2023. The quality of the articles was evaluated using guidelines, i.e., identification, review, choice and inclusion. The quality of the reviews was assessed using the measurement tool for evaluating systematic reviews. The search was performed using Boolean logical operators AND, OR and NOT. The search was performed using Boolean logical operators AND, OR and NOT Keywords such as implant abutment, implant abutment connection, external hex, internal hex and morse taper the words were used alone and/or in combination with one another to search the database. The option such as ‘related articles’ or similar articles were also used. Finally, search was performed of the references of review and most relevant papers following which everything was combined.
Implant-Abutment interface
The implant-abutment interface is the surface where the dental implant and the prosthetic abutment connect. There is more than one type of implant-abutment interface and the one selected by the practitioner often depends upon the location of the implant and the type of prosthesis that will be attached. Implant abutment connection can be external or internal. Depending on the space between connecting part they can slip fit or friction fit. While according to the angulation between connecting parts they can butt joint or beveled joint. According to geometric configuration, interface can Octagonal, Hexagonal, Conical, Cylinder hex, Spline, etc.
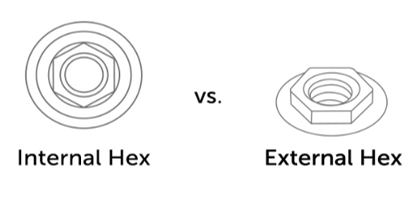
External hexagon ([Figure 1])
A connection feature that extends superior to the coronal portion of implant. The history of implant dentistry dates back to 1980s with the development of the Branemark Protocol. The original protocol was a two-stage procedure. The first stage involved the placement of a titanium screw into the bone followed by a healing period of 3 months. Stage 2 involved the exposure of the implant and attachment of a transmucosal element. Here, the implant abutment connection used was an external hexagon of 0.7mm height. [7] The external connection has served well over the years and it has been incorporated in a number of systems. This design offers a great variety of restorative options due to the interchangeability of abutments among the manufacturers. Since then implant dentistry has evolved continuously and has expanded its usage in the restoration of one or few missing teeth, maxillofacial prosthetics. The disadvantages of the Branemark external hex make it unsuitable for these applications. The original external hex lacks an effective anti- rotational device. [8] This rotational freedom of the abutment over the implant causes screw loosening which in turn leads to micro-movements during loading. In addition, when components do not seat properly, tightening a screw may damage the threads within the implant or on the screw itself. Either way the misfit of the abutment and implant leads to screw loosening. [9]
Frequency of screw loosening was more in external hex design, to overcome this various modification were introduced. To overcome the screw loosening caused by adverse force distribution and instability of the abutment connection the first change was done by increasing the width and height of the external hex connection. Currently available external hex heights range from 0.7, 0.9, 1.0, and 1.2 mm and with flat–flat widths of 2.0, 2.4, 2.7, 3.0, 3.3, and 3.4 mm, depending on the implant platform. By increasing the width and height leads to increase in the fulcrum arm and the area of abutment screw engagement also increases, thus decreases the tipping forces on abutment screws and reducing the occurrence of screw loosening. [10]
Binon reported that less than 2 degrees of rotational freedom between an implant and its abutment showed the most stable joint, and more than 5 degrees of rotational freedom resulted in dramatic decrease in the number of loading cycles needed to loosen the implant/abutment joint. [11]
One more modification that was incorporated to prevent screw loosening was applying preload.
Advantages of external hex:
Long term clinical follow-ups are available.
Compatible with multiple implant systems.
Disadvantages of external hex
Lacks anti-rotational devices.
Frequent screw loosening.
May affect esthetics.
Modifications of external hex
Tapered external hex
The hexagon connection design was introduced to improve the fit between the implant and abutment by creating a 1.5-degree tapered interface. This design reduces rotational freedom and screw loosening by interlocking the mating hexes with a frictional fit, providing increased stability. First introduced by Swede-Vent TL (Paragon Implant Co, Encino, CA), and also available in the Spectra implant system, this design aims to improve accuracy and stability. Independent studies have confirmed zero micromotion at the implant-abutment interface, highlighting the advantages of the tapered hexagon design over the traditional external hexagon. [12]
External Octagon
The external octagon design features an eight-sided implant-abutment interface that allows for 45° rotation of the abutment. [13] Due to its circular-like geometry, it provides minimal rotational resistance and is not considered very successful. This design is also incompatible with angled abutments. Commercially introduced as a narrow diameter implant (3.3 and 3.5 mm) by ITI Narrow Neck for mandibular anterior teeth, it claimed good lateral and rotational resistance and strength, though studies to support these claims are lacking. Consequently, the external octagon design is not widely favored in implant-abutment connections.
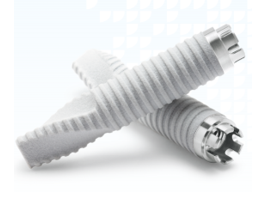
Spline implant abutment connection
Spline implant abutment connections (Fig 2), developed by Calcitek in 1992, serve as an alternative to the external hex connection. [14] This design features six spline teeth extending outward from the implant body that fit into six corresponding grooves in the abutment, creating a snug fit and providing excellent locational accuracy. [15] This connection reduces screw loosening and minimizes rotational movement compared to traditional external hex designs, leading to increased stability between the implant and abutment.
However, the spline connection's narrow diameter implants lack stability and may experience spline fractures. Available in 4, 5, and 3.25 mm diameters, the 4 and 5 mm implants offer strong mechanical stability and reduced incidence of screw loosening. In contrast, the 3.25 mm diameter implant, with its smaller splines and narrow platform, has a frail interface, making it less popular due to its vulnerability. [16]
Internal connections
Internal connections (Fig. 1) have been introduced to reduce mechanical complications from external connections and decrease stress transfer to the crestal bone. Acting as anti-rotational and indexing features, these connections improve implant stability and simplify restorative procedures. One of the first internal hex designs was introduced by Niznick in 1986. [15] This core-vent implant featured a 1.7 mm-deep hex below a 0.5 mm wide, 45° bevel, distributing intraoral forces deep within the implant and enhancing joint stability. Internal interfaces offer several benefits:
Reduced vertical height for restorative components
Deep distribution of lateral loading within the implant
Shielded abutment screw
Stiff, unified body resisting joint opening
Vibration buffering
Potential microbial seal
Flexibility and aesthetic advantages.
The internal connection implants can be divided into the following groups:
Passive fit/slip fit joint
6-point internal hex:
– Center pulse-core vent/screw vent
– Friadent-Frialit-2
12-point internal hex:
– 3i-osseotite certain
3-point internal tripod:
– Alatech technologies, Camlog
– Nobel biocare/Replace select
Internal octagon: Omniloc, Sulzer Calcitek
Friction fit
Locking taper/morse taper:
8 degree taper (ITI straumann, Avana, 3i TG, Ankylos)
11 degree taper (Astra)
1.5 degree tapered rounded channel (Bicon).
Six-point internal hexagon
The six-point internal hex is a widely used abutment fixture due to its hexagonal geometry, allowing the abutment to fit over the implant fixture at six different 60° angles. [17] The initial internal hex implant featured a 1.7 mm-deep hex below a 0.5 mm wide 45° bevel, offering a reduced vertical height platform for prosthetic attachment and better stability due to the longer hex. [12]
Various manufacturers offer this type of connection. For example, Central Pulse (Screw-vent) provides an implant with a 1.2 mm internal connection, which evolved from the original core vent implant to the tapered screw vent implant. This design distributes intraoral forces deep within the implant, enhancing joint stability compared to traditional external hexagons. [18], [19]
Another example is the Frialit-2 system from Friadent, Dentsply. It combines a cylindrical implant design with an internal connection, effectively distributing axial loads to the step plateaus and lateral forces to the enveloping surfaces. The internal hexagon connection offers 60° indexing and rotational resistance, blending the benefits of cylindrical and internal connection designs. [20]
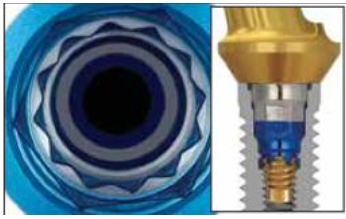
Twelve-point Hexagon
The 12-point internal hexagon (Fig. 3) design allows the abutment to be positioned in 12 different orientations at 30° intervals, making it particularly useful for angled abutments. [13] Research by Tang et al. demonstrated that this design provides better stress distribution and less displacement compared to other designs. [21]
Manufacturers market the 12-point double internal hexagon, also known as the offset hexagon, for its flexibility in abutment placement. This design, exemplified by the Osseotite Certain implant from 3i Implant Innovations Inc., offers greater freedom to correct off-axis angulations of the abutment relative to the implant.
While offering enhanced flexibility in abutment positioning, the 12-point internal hexagon design must maintain strong mechanical properties at the implant-abutment interface. Studies using finite element analysis have shown that implant systems like the reduced-diameter 3i Implant System with a 12-point double internal hexagonal connection exhibit superior stress distribution and minimal displacement compared to other designs, such as those with external hexagonal connections like the Brånemark system. [10]
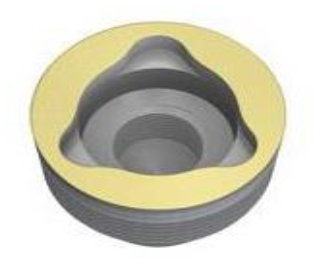
Three-point Internal Tripod
The three-point internal tripod (Fig. 4) design features a triangular internal geometry, introduced by Nobel Biocare as the Replace Select system. Available in diameters of 3.5, 4.3, 5, and 6 mm, it is color-coded for easy identification. However, its limitation to 120-degree abutment positioning makes it less clinically preferred. Studies have shown that under off-axis loading, stress distribution favors external hex connections over the 12-point double hexagon design of the Replace Select system. Consequently, this design is not widely favored for implant-abutment connections. Another example of an internal tripod system is the Camlog implant from Alatech Technologies, featuring a 5.4 mm internal connection length and claimed to provide secure, antirotational stability with its 'tube in tube' effect. [22]
Internal octagonal
The internal octagonal implant features an 8-sided internal geometry allowing the implant to be positioned over the abutment at 45-degree intervals. Introduced by Omniloc, Sulzer Calcitek, this design presented thin walls and a small diameter resembling a circular profile, resulting in minimal rotational and lateral resistance during function. However, due to these drawbacks, it is no longer marketed. [4]
Morse taper
The Morse taper implant-abutment connection (Fig. 5) design features a tapered projection from the abutment that fits into a corresponding tapered recess in the implant, creating a friction fit and cold welding at the interface. This design relies on the friction fit to prevent rotation and abutment screw loosening. [23]
The original Morse taper concept includes 2-degree and 4-degree tapers designed for a precise fit without a self-locking thread. In Morse taper connection implants, the abutment and fixture act as a single piece due to the "cold-welding" effect, eliminating microgaps and preventing bacterial leakage. The taper interface also resists lateral loading, preventing the abutment from tilting. [23]
Sutter et al. proposed the Morse taper connection as an optimal combination of predictable vertical positioning and self-locking characteristics. Norton supported this by showing that conical connections between implant and abutment significantly enhanced the system's resistance to bending forces. Further studies by Levine et al. and Felton confirmed reduced complications, such as abutment screw loosening, with Morse taper connections compared to external hex connections. [24]

Degree Morse Taper
The Morse taper or cone screw tapered connection, first utilized by the ITI group in Switzerland, aimed to create a mechanically stable, self-locking interface with a friction lock similar to those used in mechanical engineering.
The ITI-Straumann implant design evolved into the Synocta design, which added an internal hexagon to the Morse taper connection, as proposed by Wiskott and Belser. This modification allowed for the rotation and repositioning of the abutment over the implant at different angles, facilitating precise transfer of the implant position to the master cast with only one transfer system and one analog.
Osteo-Ti's Combi implant combines the features of an internal hex and Morse taper implant, offering accurate positioning and a similar friction fit. Other manufacturers marketing 8-degree Morse taper implants include Avana, 3i TG, and Ankylos. [25]
Degree
This abutment, marketed by Astra Tech, features a conical seal design that minimizes micromovement and microleakage at the implant-abutment interface. The fixture and abutment are securely connected at an 11.5-degree angle by the conical seal. The implant also includes a microthreaded conical neck and TioBlast surface. The microthreads at the top of the fixture prevent stress concentration around the alveolar ridge crest, reducing marginal bone loss.
Introduced by Bicon implants, this true Morse taper design features a 1.5° taper. Bicon claims that this taper provides a bacterial seal at the implant-abutment interface, with a microgap of less than 0.5 microns, preventing microbial leakage and reducing the risk of soft tissue inflammation and bone loss around the implant.
The Bicon locking taper abutment, which has no screw, relies on friction to maintain its integrity. Assembly involves driving the 1.5° Morse taper into the matching socket in the implant, generating a high clamping force. This force results from the relative slip between the two friction surfaces under high contact pressure, causing cold welding at the implant-abutment interface.
Discussion
This review outlines the evolution of implant-abutment connections, starting from the 0.7 mm traditional external hexagon of Branemark's implant to the development of Morse taper connections. Branemark's external hex connection was adequate for restoring a completely edentulous arch with a series of implants connected by a metal bar. However, with a better understanding of osseointegration and the refinement of surgical protocols, the applications of implant dentistry have expanded significantly.
Dental implants are now used for a wide range of applications, including restoring completely edentulous arches, partial edentulous situations, single tooth replacements, and fixed bridges. With these increasing applications, the requirements for implant-abutment connections have also grown. These connections must now provide anti-rotation and prosthetic indexing, particularly for single posterior tooth restorations, which are the most challenging to retain.[26], [16]
To address complications such as abutment screw loosening and fracture associated with Branemark's external hexagon in single tooth restorations, various design modifications have been made. These include increasing the height and flat-to-flat width of the mating surfaces. Other innovations, such as the tapered hexagon and spline dental implant, have been introduced to overcome the limitations of the external hexagon. [5]
The search for a more effective implant-abutment connection led to the development of the internal hexagon design, which has been further modified to designs such as the three-point internal tripod, 12-point internal hexagon, and internal octagon. The clinical significance of these designs lies in the freedom of positioning the abutment over the implant, which is maximum for the 12-point internal hex and minimum for the three-point internal tripod.
This review describes various commercially available implant-abutment connections, highlights manufacturers' claims, and supports them with published data wherever available. It aims to help clinicians make informed decisions about which implant system and implant-abutment interface to use, from the array of commercially available options.
Conclusion
From the given study it can be concluded that,
The implant-abutment interface is crucial for the lateral and rotational stability of the implant-supported restoration.
Internal connections generally offer better prosthesis retention and stability, reducing stress on the cervical region of the implants and retention screws.
Conical interfaces, combined with retention elements at the implant neck, minimize micromotion.
All prosthetic platforms can achieve high success rates if strict criteria for indication and limitation are followed, highlighting the importance of reverse planning to reduce implant overload.
This review has outlined the evolution of implant-abutment connections, from the traditional external hexagon to advanced internal designs.
It aims to inform clinicians about the various design characteristics and clinical applications of contemporary implant systems, helping them make informed decisions for optimal patient outcomes.
Conflict of Interest
None.
Source of Funding
None.
References
- T Albrektsson, G Zarb, P Worthington, AR Eriksson. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Imp 1986. [Google Scholar]
- D Buser, S Ingimarsson, K Dula, A Lussi, HP Hirt, UC Belser. Long-term stability of osseointegrated implants in augmented bone: a 5-year prospective study in partially edentulous patients. Int J Periodon Restor Dent 2002. [Google Scholar]
- L Gaviria, JP Salcido, T Guda, JL Ong. Current trends in dental implants.. J Korean Assoc Oral Maxillofac Surg 2014. [Google Scholar]
- PP Binon. Implants and Components: Entering the New Millennium.. Int J Oral Maxillofac Imp 2000. [Google Scholar]
- PP Binon. Implants and components: entering the new millennium. Int J Oral Maxillofac Imp 2000. [Google Scholar]
- S Gracis, K Michalakis, P Vigolo, PV Von Steyern, M Zwahlen, I Sailer. Stefano Gracis Konstantinos Michalakis Paolo Vigolo Per Vult von Steyern Marcel Zwahlen Irena Sailer. Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res 2012. [Google Scholar]
- PI Branemark. Osseointegration and its experimental background. J Prosthet Dent 1983. [Google Scholar]
- K Beaty. The role of screws in implant systems. Int J Oral Maxillofac Impl 1994. [Google Scholar]
- PC Pinheiro Feitosa, AP Barbosa De Lima. Laís Regiane Silva-Concílio, William Cunha Brandt, and Ana Christina Claro Neves Stability of external and internal implant connections after a fatigue test. Eur J Dent 2013. [Google Scholar]
- T Kitagawa, Y Tanimoto, M Odaki, K Nemoto, M Aida. Influence of implant/abutment joint designs on abutment screw loosening in a dental implant system. J Biomed Mater Res B Appl Biomater 2005. [Google Scholar]
- PP Binon. Evaluation of machining accuracy and consistency of selected implants, standard abutments, and laboratory analogs. Int J Prosthodont 1995. [Google Scholar]
- G Niznick. The implant abutment connection: the key to prosthetic success. Compendium 1991. [Google Scholar]
- MA Ronak Mukundkumar Shah, V Aras. Implant-abutment Selection: A Literature Review. Int J Oral Imp Clin Res 2014. [Google Scholar]
- RE Vogel, JP Davliakos. Spline implant prospective multicenter study: interim report on prosthetic screw stability in partially edentulous patients. J Esthet Restor Dent 2002. [Google Scholar]
- HC Hong, YM Chang, YH Pan. The Stability of Implant-abutment Complex with Different Implant-abutment Connection Designs -Review of Literature Taiwan. J Oral Maxillofac Surg 2015. [Google Scholar]
- PP Binon. The spline implant: design, engineering and evaluation. Int J Prosthodont 1996. [Google Scholar]
- DR Prithviraj, V Gupta. The Evolution of External and Internal Implant-Abutment Connections: A Review. Int Dent Res 2012. [Google Scholar]
- GA Niznick. The Core-Vent™ implant system. The evolution of the osseointegration implant. Oral Health 1983. [Google Scholar]
- GA Niznick. The implant abutment connection: The key to prosthetic success. Compend Cont Educ Dent 1991. [Google Scholar]
- G Krennmair, S Schmidinger, O Waldenberger. Single-tooth replacement with the Frialit-2 system: A retrospective clinical analysis of 146 implants. Int J Oral Maxillofac Imp 2002. [Google Scholar]
- CB Tang, SY Liu, GX Zhou, JH Yu, GD Zhang, YD Bao. Nonlinear finite element analysis of three implant-abutment interface designs. Int J Oral Sci 2012. [Google Scholar]
- CB Tang, SY Liu, GX Zhou, JH Yu, GD Zhang, YD Bao. Nonlinear finite element analysis of three implant-abutment interface designs. Int J Oral Sci 2012. [Google Scholar]
- FG Mangano, P Zecca, F Luongo. Giovanna Iezzi and Carlo Mangano Single-Tooth Morse Taper Connection Implant Placed in Grafted Site of the Anterior Maxilla: Clinical and Radiographic Evaluation. Case Rep Dent 2014. [Google Scholar]
- BR Merz, S Hunenbart, UC Belser. Mechanics of the implant- abutment connection: An 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Imp 2000. [Google Scholar]
- TA Ding, RD Woody, FL Higginbottom, BH Miller. Evaluation of the ITI Morse taper implant/abutment design with an internal modification. Int J Oral Maxillofac Imp 2003. [Google Scholar]
- T Kallus, C Bessing. Loose gold screws frequently occur in full arch fixed prostheses supported by osseointegrated implants after 5 years. Int J Oral Maxillofac Imp 1994. [Google Scholar]
- Introduction
- Search strategy
- Implant-Abutment interface
- External hexagon ([Figure 1])
- Advantages of external hex:
- Disadvantages of external hex
- Modifications of external hex
- Spline implant abutment connection
- Internal connections
- Six-point internal hexagon
- Twelve-point Hexagon
- Three-point Internal Tripod
- Degree Morse Taper
- Discussion
- Conclusion
- Conflict of Interest
- Source of Funding
How to Cite This Article
Vancouver
Valvi NN, Khalikar S, Mahale K, Rajguru V, Mahajan S, Tandale U. Evolving interfaces: A comprehensive review of implant-abutment connections [Internet]. Int Dent J Stud Res. 2025 [cited 2025 Sep 07];12(3):123-129. Available from: https://doi.org/10.18231/j.idjsr.2024.024
APA
Valvi, N. N., Khalikar, S., Mahale, K., Rajguru, V., Mahajan, S., Tandale, U. (2025). Evolving interfaces: A comprehensive review of implant-abutment connections. Int Dent J Stud Res, 12(3), 123-129. https://doi.org/10.18231/j.idjsr.2024.024
MLA
Valvi, Nikita Narendra, Khalikar, Smita, Mahale, Kishor, Rajguru, Vilas, Mahajan, Sonali, Tandale, Ulhas. "Evolving interfaces: A comprehensive review of implant-abutment connections." Int Dent J Stud Res, vol. 12, no. 3, 2025, pp. 123-129. https://doi.org/10.18231/j.idjsr.2024.024
Chicago
Valvi, N. N., Khalikar, S., Mahale, K., Rajguru, V., Mahajan, S., Tandale, U.. "Evolving interfaces: A comprehensive review of implant-abutment connections." Int Dent J Stud Res 12, no. 3 (2025): 123-129. https://doi.org/10.18231/j.idjsr.2024.024
