Introduction
Root resorption is a naturally occurring physiological phenomenon in deciduous dentition which eventually leads to their exfoliation in anticipation of the arrival of its permanent successor. External apical root resorption (EARR) of permanent teeth is an uncommon and frequent sequel to orthodontic tooth movement, since mechanical forces used during orthodontic treatment for various types of tooth movement may cause apical root resorption. Extensive root resorption present before orthodontic treatment may contraindicate orthodontic treatment and its occurrence during treatment, may demand the stoppage of treatment, or make the orthodontist arrive at a compromised treatment. Though the occurrence of apical root resorption occurs in individuals who have never undergone orthodontic tooth movement, the incidence among treated individuals is seen to be significantly higher. Though orthodontic tooth movement is the primary cause, various factors like individual susceptibility, systemic factors, appliance type, tooth movement, and force applied, play a major role. Most studies 1, 2, 3 agree that the resorption process ceases once the active treatment is terminated and the reparative processes take over. Root resorption typically attacks the tip of the root and travels coronally, seeming to what has been termed a "shed roof' effect on the root. The area nearer to the pulp (away from PDL) is the last to give way. This process is exactly opposite to the process of tooth formation, resorption is taking place instead of formation. Orthodontic root resorption is common, but clinically significant root resorption is fortunately rare. At any time when there is an injury to the periodontal ligament or pulp, causing inflammation, resorption of the root surface may occur. In the same context, the functional and aesthetic corrections gained from orthodontic treatment far outweigh the concurrent side effects of root resorption.
Types of root resorption
Since tooth resorption may begin either on the external surface or inside the tooth i.e on pulpal reaction, it can be broadly divided into
Over the years various authors 4, 5, 6, 7 have classified root resorption into various types owing to the type of involvement, etiology, or any other factors.
Andreasen (1985) 8 has classified external root resorption into three main types according to etiology and pathogenesis.
Surface resorption - caused by injury to periodontal ligament
Inflammatory resorption - caused by combined injury to the periodontal ligament and possibly to the root surface, and also there are bacteria present in the root canal.
Replacement resorption- osteogenic bone grafts are placed close to the root surface, then the osteogenic healing process may overwhelm the periodontal ligament repair process and ankylosis occurs with fusion between adjacent bone and root surface
According to Brezniak and Wasserstein 9, Orthodontically induced root resorption can be classified as
Cemental or surface resorption with remodeling: Only the outer cemental layers are resorbed, and they are later fully regenerated or remodeled.
Dentinal resorption with repair (deep resorption): Cementum resorption along with resorption of the outer layers of the dentin and usually repaired with cementum material.
Circumferential apical root resorption: Full resorption of the hard tissue components of the root apex occurs, and root shortening is evident.
It is important to distinguish between the two types (location) of external root resorption because what may be true in the former may not necessarily be so for the latter. This distinction must be made clear when interpreting the literature.
Etiology of root resorption
The etiology of root resorption may be due to several factors alone or in combination with each other.
Root resorption may occur as a result of:
Dental trauma
Surgical procedures
Infections
Ectopic eruption of adjacent teeth
Orthodontic treatment
Loss of bony support
Pressure from tumors/cysts
Irritation from chemicals (Eg. H2O2 during bleaching)
Idiopathic
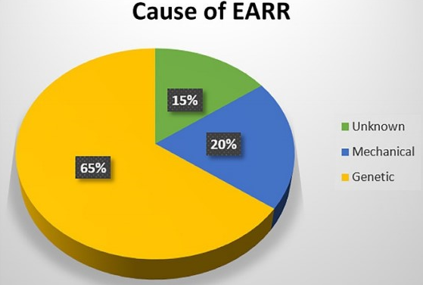
Etiologic has been divided by authors 10, 11 into mainly three categories;
Systemic factors – Including genetic factors, ethnicity, chronological and dental age, nutrition and other factors
Local factors – Any deviation from normal of dental and surrounding tissues, like occlusal trauma, endodontically treated teeth
Treatment-related factors- include factors occurring due to treatment procedures, like duration and direction of treatment, magnitude of treatment, mechanics, appliance type or any extraction protocols. (Figure 1)
Mechanism of root resorption
The initiation of resorption depends on barrier alterations. Thus the osteoclasts always appear on a raw bone surface unprotected by the barrier. Development of root resorption seems to be an interrelationship between temporary damage of tooth surface barrier and general resistance against resorption and remodeling of alveolar bone.
Root resorption occurs mainly due to local injury of the periodontal membrane with the development of sterile coagulation necrosis i.e. hyalinization. It is related to signals or damage to the cells and other barriers that protect the root surface. If the force placed on a tooth exceeded the capillary blood pressure, the capillary would collapse, cut off blood circulation, and lead to areas of tissue necrosis and thus root resorption. 12 It is thought that when resorption processes exceed the reparative capacity of cementum orthodontic induced root resorption (OIRR) will ensure. OIIR starts along the circumference of the main necrotic hyalinised tissue and continues inwards for a few days, till the removal of the main hyalinised zone.
It is suggested that the cementoid layer acts as a defence against resorption describing it as a resorption-resistant “coating”. 13 The cementum is continuously deposited throughout life, while the alveolar bone is constantly being remodeled which results in osteoclasts being the part of normal cell environment of the bone surface. 14 The higher turnover rate of the bone side results in the tissue being newer and more immature than adjacent to the cementum, which means the cementum is surrounded by more mature collagen which is more resistant to chemical changes than bone, therefore cementum is more resistant to resorption.
There are mainly two different cell populations that are involved in the root resorption process. The cells in the initial phase of resorption (1-3 days) are not odontoclasts as they lack tartrate-resistant acid phosphatase (TRAP) enzyme, they are macrophage–like cells whose role is to eliminate the necrotic tissues. After the first 3 days, the initial phase of cells is followed by multinucleated (odontoclasts) as well as mononucleated TRAP-positive cells which invade the hyalinised tissue from the periodontal membrane as well as the adjacent alveolar bone. They attack the cementum and eventually dentine. Kvam15 was the first to describe resorption lacunae which penetrate the cementum into dentin in human teeth. The surface of the root present under the main hyaline zone resorbs several days later. This resorption process of the root and the repair process in the periphery continues at the same time. The process stops when there is no hyaline tissue remaining and/or the force level decreases. 16 Rudolph 17 observed resorption usually starts from the root tip and travels towards the coronal region, making what has been termed a “shed roof” effect on the root.
The reason for the apex being more affected than the cervical or middle thirds of the root is,
Forces applied are concentrated on the apex
It is made of cellular cementum which is less mineralized and easily resorbed
Also, compression & decrease in the width of the PDL affects the apex more than it affects the cervical or middle third.
The role of exposed dentin
Possible involvement of the pulp through the apices
Multiple foramina and complicated surface anatomy
Stresses applied on the neurovascular bundle exiting the pulp
EARR can be defined operationally as the degree a root has shortened from its original ( or expected ) length by clastic activity. Broadly, two methods have been used to quantify resorption
Ratio scale data
Measurements with calipers or some computer-aided device
Levander and Malmgren (1988) 18 classified root resorption as:
Grade 0 No root resorption
Grade 1 Mild resorption. Root with normal length and only irregular contour
Grade 2 Moderate resorption. A small area of root loss with the apex having an almost straight contour
Grade 3 Accentuated resorption. Loss of almost one-third of root length
Grade 4 Extreme resorption. Loss of more than one-third of root length
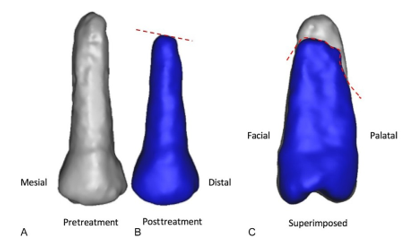
The diagnosis of root resorption can be made by a variety of methods which include diagnosis and laboratory diagnosis. There have been attempts to reproduce three-dimensional structures from a two-dimensional film. These techniques are known as laminography or focal plane tomography. It involves translating an object/subject together with the detecting medium in such a way that only one narrow slice parallel to the translation plane is in focus. With the advent of digital computers, an approach called computer tomography became possible, by taking several slices, a three-dimensional map is produced.
Microcomputer tomography can be taken for investigations without damaging or removing any material. This system is therefore useful for viewing biological structural materials such as calcified tissues. The SkyScan micro tomography uses a non-destructive procedure to create a three-dimensional reconstruction of the objects’ inner structure from two-dimensional X-ray shadow projections. The software package, VG Studio Max v1.2 is used to collate all the axial slices to form a three-dimensional reconstruction of the scanned image. This software package also has the function of removing the bony tissue around the scanned tooth, which facilitates the viewing of any defects on the cemental surface. 19
Cone-beam computed tomography (CBCT) is a new radiographic method with several applications in various diagnostic areas. The great advantage of this technology is to offer 3-dimensional (3D) imaging of dental structures and provide clear images of highly contrasted structures, such as bone. Compared with conventional computed tomography, CBCT technology in clinical practice has important advantages such as minimization of the radiation dose, image accuracy, rapid scan time, fewer image artifacts, chair-side image display, and real-time analysis. (Fig 2)
Laboratory diagnostic techniques include histological methods like:
Light microscopy- is used to quantitatively analyse root resorption craters, but this technique could not account for the variation in size, shape, and depth of the craters and variation in root morphology and consequently, accurate quantitative measurements of these craters could not be achieved. 20
Transmission electron microscopy- While TEM images provide useful 2D images they are not designed to easily produce 3D reconstruction of specimens.
Scanning electron microscopy- SEM provides an overall image of resorption craters on the root surface with minimal tissue preparation. SEM images have been used to assess root resorption craters in 2 dimensions. 12 This method is highly accurate and reproducible. However, this method is time-consuming and difficult to perform for large samples.
Repair of root resorption craters begins or starts, when the force applied is discontinued or reduced below a certain level. This has been recorded to begin as early as the first week of retention. The reparative process increases with time, especially during the first 4 weeks of retention. 21 However, by the 5th and 6th weeks, repair seems to slow and reach a steady state. After 10 days of cessation of tooth movement, the multinucleated resorptive cells and collagen-producing fibroblast-like cells occupy the same resorption lacuna. The fibroblasts invade the lacunae from the circumference indicating a transition of resorption to repair. Approximately two weeks after the force is removed, different phases of repair can be observed with the placement of new cementum or coverage of root dentine with structures. By three weeks from the start of the repair process, the mineralized cementum fills the resorption lacunae, and PDL attachment is restored.
The possible repair level in resorption cavities that can be histologically observed can be summarized as follows: 20
Partial Repair: Part of the surface of the resorption cavity is covered with reparative cementum (cellular or acellular cementum).
Functional Repair: The total surface of the resorption cavity is covered with reparative cementum without the re-establishment of the original root contour (cellular cementum).
Anatomic Repair: The total surface of the resorption cavity is covered with reparative cementum to an extent such that the original root contour is re-established.
The clinician must be conscious of the possible risk factors that may predispose to root resorption. Risk factors can be broadly classified under three groups:
General factors - These factors are directly related to the patient, and may or may not be influenced by the patient and may be either genetic or environmental in origin. Factors like gender, ethnicity, age, nutrition, endocrine imbalances, or any other factors may predispose to the development of root resorption.
Dental factors – Various authors have evaluated abnormalities in root shape and their association with the resorptive process. Among differently shaped root ends the least resorption was observed in blunted root ends22 and the greatest was seen in pointed or tapered root ends. Other dental factors include tooth specificity, surrounding tissues, and previous orthodontic history
Mechanical factors - These factors are attributed to the mechanics of orthodontic therapy and are controlled by both the clinician and the patient. The type of tooth movement performed, and the duration of force application magnitude of force, as well as rigid fixation of the arch-wire with brackets or the use of full-size rectangular wires in bracket slots, could be the most important factors predisposing a tooth to the resorptive process.
Several publications described a positive correlation between increased force levels and increased root resorption, as well as between increased treatment time and increased root resorption. Clear aligners apply intermittent forces to the teeth such as many active removable appliances. It has been proposed that the pause in treatment with periodic force allows the resorbed cementum to heal and prevent further root resorption.
Segal et al. reported that a long treatment duration contributes to severe EARR in fixed aligner treatment. However, though the velocity of tooth movement by clear aligner therapy (commonly 0.2 mm every 10-14 days) could be slower than by fixed appliance treatment (generally 1 mm per month), it might cause less EARR. 11 Moreover, the root resorption that was observed and measured using 3D data was 13.34 mm3 in tooth volume loss. The highest amount of root resorption was observed in the maxillary central incisors. 23 There is no clear evidence-based answer to the relationship between root resorption and orthodontic treatment with clear aligners. Current evidences suggest that clear aligners might not avoid root resorption, but the incidence and severity of resorption could both be lower compared with results reported by treatment with fixed appliances.
Prevention and management of root resorption
Steps in the management of root resorption should follow mainly,
Imaging: Initial periapical 24 or limited CBCT is essential in adult patients to properly examine the root morphology and location of the roots with clarity. History: A careful history may suggest a possible etiology for root resorption. If a patient is at higher risk, especially for families, specific documentation of this additional level of risk must be included in the informed consent for treatment.
Progress Review: Documenting the progress for all cases is good clinical practice, but particularly important if risk factors for EARR
Before the start of orthodontic treatment, it is ideal to inform the patient regarding the possible risk factors rather than to later apologize. It is obvious if the orthodontist decides to initiate treatment after reviewing all of the relevant data collected, the expected esthetic and functional benefits far outweigh the minor root changes observed in most patients. From a medico-legal point of view, the importance of diagnostic records and thorough evaluation of them should not be overlooked. The decision whether to continue active tooth movement depends upon planned further movement of the tooth, and the amount of resorption visible on the radiograph at the particular stage. It must be noted that there are no consensus standards on what constitutes severe EARR. If root resorption is noticed in progress visits, a temporary halt in orthodontic treatment for a period of 4 to 6 months is suggestable.25 In this period the resorptive process ceases and the reparative process starts. Ideally, the tooth should not be in hyperfunction, and no force applied,26 this usually means the placement of a passive archwire to hold the teeth exactly where they are. After this rest period, treatment can continue. If severe root resorption exists where the EARR is more than 4 mm is encountered midtreatment, the usual procedure is to discontinue appliance therapy. Alternative approaches for treatment must be chosen (either surgical or extraction/prosthetic). Appropriate follow-up and necessary counseling should always accompany this approach.
The effect of hormones and cytokines in reducing resorption has been identified by previous studies. The main hormone attributed to this was L-thyroxine. 27 It is assumed to increase the resistance of cementum and dentin elastic activity. The major cytokine found in correlation with the resorptive process was prostaglandin E2. 28 Though the previous studies confirmed its role in the process, a recent evaluation demonstrated little or no effect for this cytokine on either the depth or the number of resorption lacunae found in resorbed tooth roots. A recent report by Bialy et al. 29 evaluated the effect of low-intensity pulsed ultrasound (LIPUS) on the healing process of orthodontically induced root resorption in humans. They found a significant decrease in areas of resorption and the number of resorption lacunae in teeth exposed to LIPUS. The result of this study is encouraging, as it demonstrates a non-invasive method to reduce root resorption in humans.
Discussion
Long-term evaluation of resorbed tooth roots
The original root contours and length are never re-established, but the function of the tooth apparatus is not severely affected. The main problem cited for these teeth on a long-term basis is their reduced suitability as abutments for prosthetic replacements, because of their less favorable crown/root ratio. 30 These teeth will be less resistant to trauma and have higher rates of marginal periodontitis, which can make their prognosis critical. Generally, EARR stops completely with the cessation of active forces. Over time a “smoothing” of rough surfaces has been observed by clinicians
EARR is an undesirable complication of orthodontic tooth movement. The orthodontist must be aware of root resorption because even though no direct cause has been proven, orthodontic treatment has been identified as one of the most commonly associated factors. By far, there is no consistent evidence for the precise identification of the orthodontic patient that will develop root resorption, orthodontists should keep in mind the various indicators known and promote systematic radiographic to monitor their patients. To individualize the diagnosis and treatment plan could mean the difference between the success and failure of orthodontic treatment.
Conclusion
The orthodontist must be aware of root resorption because even though no direct cause has been proven, orthodontic treatment has been identified as one of the most commonly associated factors. By far, there is no consistent evidence for the precise identification of the orthodontic patient who may develop root resorption, orthodontists should keep in mind the various indicators known and promote systematic radiography to monitor their patients. To individualize the diagnosis, the possible risk factors for root resorption and treatment plan could mean the difference between the success and failure of orthodontic treatment. Mechanical forces and other environmental factors do not adequately explain the variation seen among individual expressions of root resorption. Extensive clinical research is required to gain a deeper knowledge of the aetiology and pathogenesis of the various types of root resorption.