Introduction
Fibroma is a reactive hyperplasia of fibrous connective tissue that develops from local irritation or injury; it is not a true neoplasm.1 An inflammatory hyperplastic lesion that can form from almost any soft-tissue site including the tongue, gingiva, and buccal mucosa at any age can heal into a traumatic or irritant fibroma.2 Gingival fibroma is clinically characterized by steady, well-demarcated growth that is typically accompanied by a sessile or pedunculated base, smooth and a hard consistency that makes speech and chewing difficult. There is a female predilection for gingival fibroma, which is most common in the 3rd to 5th decades of life.3 The lesion appears as a broad-based, round or ovoid, painless swelling that appears lighter in color compared to the neighbouring tissue because of decreased vascularity.4
Fibromas are treated by completely excising the lesion surgically with a scalpel, electrocautery, and lasers. Recurrence rate of irritation fibromas is uncommon, however it can happen if the irritant is not completely eliminated. 5 About 60% of irritant fibromas are located in the maxilla, and are mostly seen in the anterior region, presenting in the incisor-cuspid region 50-60% of the time and are rare in the posterior region. 6 In the present case report, the traumatic fibroma was found in the posterior teeth region of mandible in a male patient. This case report describes the investigations, histopathogical findings, diagnosis, and treatment of irritation fibroma.
Case Report
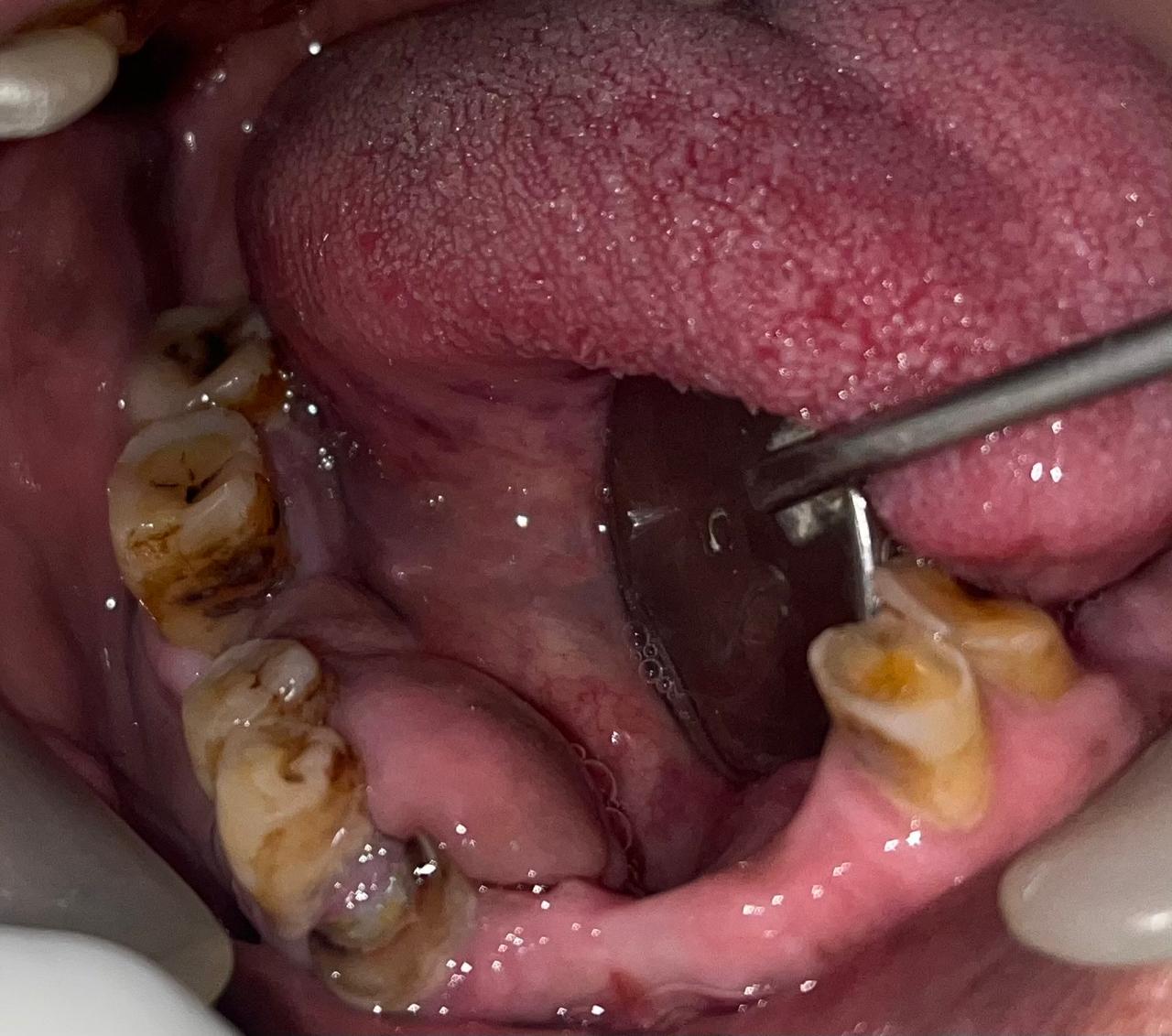
A male patient, 60 years old, came to the periodontics department complaining of swelling from last one year in the lingual vestibular area of his right mandibular posterior region which was increasing in size. With no prior history of discomfort, paresthesia, or bleeding, the growth gradually grew to its current size. The lesion was painless when palpated, and no trauma was found to the soft or hard tissues. The patient was having significant medical history with diabetes and hypertension. A thorough intraoral clinical examination identified a distinct, smooth-surfaced, multilobulated, exophytic growth in the lingual vestibular region of the mandibular right posterior teeth region. The growth measured about 4cm × 2.5 cm × 1.5 cm and extended mesiodistally from the distal surface of the right lower lateral incisor to the mesial surface of the right second molar (Figure 1, Figure 2, Figure 3, Figure 4). The provisional diagnosis of traumatic fibroma was made based on the clinical examination and history. The differential diagnosis, which would be confirmed by biopsy, included gingival cysts, papillomas, hyperplastic fibromas, peripheral giant cell granulomas, peripheral ossifying fibromas, pyogenic granulomas, and papillomas. 7
Investigations and treatment plan
Before investigations and surgical treatment, written informed consent was taken. All routine hematological testing, such as blood sugar levels,complete blood count, HIV screening tests, and HBsAg were within normal ranges. To exclude the possibility of calcifications, an occlusal radiograph was taken. There was no evidence of bone involvement on the radiograph. Then, an incisional biopsy of the growth was performed under local anesthesia. The specimen was put in a container with 10% formalin solution as soon as possible and sent for histopathological examination.
A keratinized stratified squamous epithelium with varied acanthosis, elongation, and papillomatosis was found in the histopathological report of the incisional biopsy (Figure 2). Dense collagen bundles, scattered chronic inflammatory cells, and blood vessels were also seen in the underlying fibrocellular connective tissue stroma. After considering these clinical, radiological, and histological results, a definitive diagnosis of traumatic fibroma was made.
The standard course of treatment for traumatic or irritating fibromas is complete excision. Thus, the treatment plan was made to surgically remove the lesion completely. Since patient was elderly, hypertensive with diabetes and after getting all biochemistry evaluation and physician consultation, it was decided to remove the lesion with laser. There are numerous advantages of laser treatment including fast action and no need for of sutures and flaps. Before surgical excision, phase I therapy included supragingival scaling and rinses with chlorhexidine mouthwash two times daily for one week. The surgical site was treated initially with topical anesthetic drugs (2% lignocaine and 1:80,000 adrenaline), and then local anesthetic infiltration was done.
Once anesthesia was determined to be effective,the fibroma was excised using a diode laser using the following settings : 5W continuously while maintaining a 400mm surgical tip in contact with the tissue and the fibrous tissue was excised (Figure 3). The tip was always in touch with the tissue, moving in oscillating patterns until the tissue was completely removed. To prevent the blood supply from collapsing, the lesion was carefully closed with an Adson clamp. To compare the surrounding tissue, the excision was performed 1 mm beyond the boundary of the lesion. There was no bleeding throughout the procedure
Postoperative instructions were provided, along with prescriptions for the antibiotic amoxicillin (500 mg) 3 times a day for 5 days and the NSAID, paracetamol 3 times a day for 3 days in order to prevent infection and pain following surgery. The patient was recalled for re-evaluation after 1 day, 15 days, 2 months and 6 months, respectively. On the first postoperative day, there was some pain and swelling that disappeared as long as the medication was taken. There was no delayed bleeding during the postoperative phase. After 15 days, soft tissue showed initial healing with minimum discomfort and slight different colour from mucosa. At 2-month follow-up, lesion was approximately healed with no discomfort. Then follow-up after 6 months, soft tissue showed complete healing with normal colour to mucosa [Figure 5, Figure 6, Figure 7, Figure 8].
Discussion
Localized fibrous tissue overgrowths are frequently observed in the oral cavity and can be difficult for clinicians to diagnose. An irritation or traumatic fibroma is an exophytic soft tissue growth in the oral mucosa. Usually, the cause of an irritation fibroma in the oral cavity is an irritant by any source. Irritation fibromas typically show up clinically as a hard, asymptomatic nodule with a smooth, pink or flesh-colored surface. It has also been referred to as fibrous polyp, fibroepithelial polyp, focal fibrous hyperplasia, localized hyperplasia, irritation fibroma, and traumatic fibroma. 8
A nodular growth made of dense collagenized fibrous connective tissue is the histological characteristic of irritation fibroma. Because of persistent inflammation, the epidermis exhibits hyperkeratosis and hyperplasia. In connective tissue, there is focal hyperplasia of mature fibroblasts and dense collagen fibers, with little to no infiltration of inflammatory cells.9 Various treatment modalities have been employed for excision, based upon clinical and anatomical factors. These consist the utilization of a traditional scalpel, cryosurgery, electrosurgery and ablation using various kinds of lasers. 10
Sharp bone spicules, calculus, foreign bodies, overhanging restoration margins, and overextended borders of the appliances are some of the traumatic irritants that can cause traumatic fibroma. The current case report describes the management of irritation fibroma, which includes the removal of any irritant, scaling of neighboring teeth, and complete aggressive surgical excision utilizing a diode laser. 11 Recurrences are uncommon and may result from repeated traumatic irritation to the same area. Additionally, there is no chance of malignancy with this lesion. 12
Electrosurgery has been utilized in dentistry to perform soft tissue sugeries. Its primary benefit is the coagulant action, which creates a region with no bleeding and improves vision in the surgical area. The process of making an incision releases thermal energy, which may be lost by diffusion into nearby tissues or in circulating blood . This could result in a thermal lesion to nearby tissues, which might retard healing or enhance the possibility of wound dehiscence. 13 Additional drawbacks include the requirement for anesthetics, reduced tactile sensitivity, an unpleasant odor, and the inability to be used in patients who have pacemakers or osteointegrated implants. 14
Since Maiman introduced the ruby laser for the first time in 1960, the application of lasers in dentistry has increased. Clinical benefits of dental lasers include decreased bleeding, a decreased requirement for anesthetics, and a reduction in postoperative discomfort and inflammation because they seal blood and lymphatic channels. 15
In 1999, diode lasers were first used in dentistry. Because of its compact size and convenience of use for soft tissues in shorter procedures, the diode laser has gained a lot of popularity in the dental field. Diode lasers operating in continuous or pulsed modes with wavelengths between 810 and 980 nm have been considered as a potential tool for oral soft tissue surgery. The oral mucosa lesions are treated using an excision approach or by ablation/vaporization methods based on the photothermal action of diode laser. 16, 17
Diode laser systems have been shown to be safe and effective in treating gingival hyperplasia, fibromas, frenectomy, epulis and vascular lesions. A significant reduction in postoperative pain has been observed in the first 24 hours following surgery when the diode laser is compared to electrosurgery. 10, 18
Conclusion
This case report shows that surgical excision of traumatic fibroma using a diode laser was shown to be a simple, effective, and affordable treatment for a large traumatic fibroma. Furthermore, there are no risks about bleeding during surgery and postoperative complications. For adequate diagnosis, histopathological findings should also be evaluated to rule out other lesions with similar clinical features.
Traumatic or irritation fibroma usually occurs due to a local irritating factor that can be managed by surgical excision and removal of the irritant.