Introduction
Localized hyperplastic lesions of the gingiva or “Epulides” as they are commonly known, are a well recognized entity since generations. Greek words "epi" and "elon" are the source of the term "epulis," which means "on the gingiva." Thus, it stands to reason that any lesion that develops on the gingiva can be clinically described using this phrase. However, this phrase does not provide any information regarding the type of lesion.1, 2
Because the lesion is not strictly speaking a granuloma and does not contain pus, the label "pyogenic granuloma" is misleading. Roughly one-third of the lesions are caused by trauma, and poor oral hygiene may also play a role.3
The most prevalent development that resembles an oral tumor is called a pyrogenic granuloma. Most, if not all, fibromas are reactive localized fibrous hyperplasias caused by trauma or local irritation, despite the word's suggestion of a benign tumor.
Although the pathophysiology and clinical presentation of this entity are better described by the phrase "focal fibrous hyperplasia," it is not often used. Pyogenic granuloma is a hyperactive benign inflammatory lesion that primarily affects females with high steroid hormone levels on their mucosa. The majority of people concur that female sex hormones play a critical role in the pathogenesis of this illness. 3 It is a development that resembles a tumor and is believed to have neoplastic origins. It typically originates around the anterior teeth in the skin or oral cavity 4. It typically arises in response to a range of stimuli, such as hormonal fluctuations, mild local irritation 5 traumatic injury, and specific medication classes. 6, 7
Case Report
A 24-year-old female patient arrived at the K.D. Dental College and Hospital Mathura's periodontology department with the main complaint of swelling in the upper front tooth region of her jaw that had been present for a year and was steadily getting bigger. Upon clinical examination, there was a 10 mm × 8 mm localized gingival edema in relation to 11,12 that was obviously inflammatory (Figure 1).
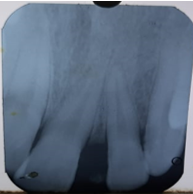
The lesion appeared as a small erythematous papule on a pedunculated base, and upon probing the region, there was spontaneous bleeding. The swelling was a smooth exophytic lesion. With the exception of the patient experiencing some minor discomfort from the growth, the lesion was painless and asymptomatic. Upon physical examination, there was no cervical lymphadenopathy or other abnormalities found. Upon analysis of the hard tissue, teeth with an atraumatic occlusion in relation to 11,12 were found. Along with moderate gingivitis, there was moderate supra- and subgingival calculus. (Figure 1). prior to surgery. (Figure 1). I.O.P.A. radiograph that displays.
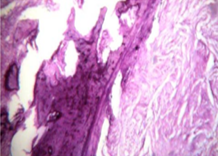
The patient’s medical history was uneventful. Thus, based on all of the a formentioned characteristics, a tentative diagnosis of pyogenic granuloma was established, and an excisional biopsy was scheduled. First, a traditional non-surgical therapy involving root planning and complete mouth scaling was carried out. The patient was instructed to brush twice a day and use a 0.2% chlorhexidine mouthwash twice a day in order to maintain good oral hygiene. After two weeks of observation, the growth gradually decreased (Figure 3). After that, the decision was made to proceed with surgical treatment of the lesion. The diaod laser was used to remove the larger localized lesion following local anesthetic as shown in (Figure 5). By excised away the remaining soft tissue next to the tooth (Figure 6), it was made sure the lesion was totally removed and prevented to recur. For one week, analgesics and antibiotics were provided. A histological study of the removed tissue was sent (Figure 7). At last, a histology report was used to make the diagnosis of pyogenic granuloma (Figure 8). The patient was recalled every month for a checkup. Two weeks later (Figure 9), there was not any noticeable clinical growth. It was completely removed. In order to preserve periodontal health and evaluate this area, supportive periodontal maintenance was recommended every three months. Even after six months, there was no return of the condition. After a year, the gingival tissue lesions had healed well and showed no signs of recurrence (Figure 10).
Discussion
An inflammatory hyperplasia that affects the oral tissues is called a pyrogenic granuloma. The first description of a pyogenic granuloma in English literature dates back to Hullihen's 1844 report. Hartzell didn't even coin the name "pyogenic granuloma" until 1904. 8 All agree now that a little injury or any underlying irritation can cause an emasculated localized connective tissue reaction. what caused this lesion to arise. 9 Calculus, bad dental care, general infections, overhanging restorations, biting one's cheek, etc. are some examples of the irritating factors. This inflammation leads to the proliferation of granulation tissue and hyperplastic growth of the underlying fibrovascular connective tissue, ultimately leading to the formation of a pyogenic granuloma.10 While pyrogenic granuloma can occur in any age group, young adult females in their second decade of life are most likely to acquire it.11 The vascular actions of female hormones could be the cause of this. The tongue, lips, buccal mucosa, and gingiva are the next most often afflicted areas.8 When a pyrogenic granuloma is removed along with its base and all associated causes are eliminated, it generally does not recur. Vilmann et al. report that only 15% of pyogenic granulomas are located on the alveolar portion of the gingiva, with the bulk of tumors finding near the gingiva's edge.4 Studies on people in Singapore have shown that the second decade of life has the highest frequency of pyogenic granuloma (Zein RB et al., 2012).12
A pyogenic granuloma is commonly observed clinically as a smooth or lobulated exophytic lesion with a sessile or pedunculated base. A pyrogenic granuloma may be a few millimeters to several centimeters in size, but they are rarely more than 2.5 cm. A significant number of pyogenic granulomas grow quickly and become big in size. 13, 14 Pyogenic granuloma treatment involves a total surgical resection.8 Pyogenic granuloma recurrence following excision is a known problem that can be avoided. Pyogenic granuloma is reported to return in 16% of treated lesions; hence, re-excision of such lesions may be required. 8
Conclusion
It is possible that the inflammatory tissue crossed the line from normal gingivitis to the development of granulomas due to a combination of different etiological variables. The lesion did not hurt because nerves do not grow within the reactive hyperplastic tissue. One effective therapeutic option for reducing the likelihood of a lesion recurrence is surgical excision. Therefore, appropriate treatment planning and a correct diagnosis should also be taken into account. The mucogingival complex should be preserved and improved while the lesion is carefully managed.