- Visibility 330 Views
- Downloads 25 Downloads
- DOI 10.18231/j.idjsr.2023.032
-
CrossMark
- Citation
Silver diamine fluoride – ‘The silver bullet’ in pediatric dentistry: An overview of past, present and prospects
Introduction
Dental caries in pediatric patients, commonly referred to as "early childhood caries" (ECC), pose a significant challenge, especially among children under 6 years old. ECC is a prevalent issue worldwide, particularly affecting vulnerable and underserved populations.[1] It is characterized by the presence of decayed, missing, or restored teeth in primary dentition. Untreated ECC can lead to numerous adverse consequences, including an increased risk of caries in both primary and permanent teeth, missed school days, pain, infections, costly emergency treatments requiring general anesthesia, and hindered growth and development.[2] Moreover, children with severe ECC are more likely to develop dental caries in their permanent dentition.[1], [2] Therefore, addressing ECC is crucial for improving overall oral and general health.
Preventive measures such as fluoride varnish, fluoridated toothpaste, and atraumatic restorative treatment (ART) have proven effective in managing ECC.[3] However, untreated caries and limited access to dental services remain significant public health issues in developing and undeveloped nations. Furthermore, behavioral management techniques and the use of non-invasive methods like cavity preparation with sharp excavators can help reduce dental fear in children and promote positive attitudes toward oral health care.[4]
"Arresting" caries involves halting the progression of the disease. This can be achieved through efficient biofilm removal and preventing the accumulation of pathogenic microbes.[5] While treating dental caries presents challenges, prevention is preferable to interception, especially in resource-constrained settings.
Preventive approaches encompass pit and fissure sealants, topical fluorides, antimicrobial agents, and dietary modifications. Chemical agents, particularly fluorides, are effective in reducing plaque levels and inhibiting bacterial growth.[3] Fluorides enhance enamel resistance to acidic challenges, inhibit bacterial metabolism, and interfere with enzyme activity in cariogenic bacteria. Fluoridation of water, milk, and toothpaste has significantly reduced dental caries incidence.[6] Various fluoride-containing topical agents like sodium fluoride (NaF), acidulated phosphate fluoride (APF), Silver fluoride (AgF), and Silver diamine fluoride (SDF) have also been developed to prevent and intercept dental caries, particularly in children.[7]
Overall, ECC is a significant public health concern among pediatric patients, with preventive measures like fluoride treatments playing a crucial role in managing and reducing its impact, especially in vulnerable populations and developing nations. The present literature review discusses the advent of SDF as an effective modality with various practical utility in pediatric dental practice.
Historical Aspect
The earliest known medicinal use of silver dates back to around 1000 BC. Silver nitrate's effective antimicrobial properties were first demonstrated by Von Naegeli.[8] In ancient times, silver found its initial use related to teeth in dental cosmetics, notably with Japanese women practicing 'Ohaguro' by blackening their teeth to indicate marital status.[9] In 1891, Stebbins showcased the inhibition of caries using a combination of silver amalgam and nitric acid on carious teeth.[10] A similar effect was achieved by directly applying silver nitrate to caries lesions, known as "Howe's solution."[11] Craig et al. reported that the AgF solution was used in dentistry as early as the 1980s.[12] A similar compound, SDF, has been accepted as a therapeutic agent by the Central Pharmaceutical Council of the Ministry of Health and Welfare in Japan for dental treatment since the 1960s.[13] A solution of 38% SDF was also used in China to arrest caries. Also, a few dentists in Southern California used SDF to arrest dental caries of young children with early childhood caries.[14] Community projects using SDF to arrest caries were planned for Cuba, sub-Saharan Africa, and several African countries.[15] While relatively new to North America, SDF has been used in certain Asian countries, including Japan and China, since the early 1970s as a caries-arresting and anti-hypersensitivity agent. Japan's Central Pharmaceutical Council of the Ministry of Health and Welfare established SDF as a therapeutic agent for dental treatment.[16] However, SDF did not gain widespread popularity outside Japan until the late 1970s.
Over the past few decades, SDF has been utilized in Australia and China to prevent dental decay. It has also been incorporated into community dental health programs in various countries, including Argentina, Brazil, Spain, and some sub-Saharan African nations. A report in 1995 detailed the use of SDF by healthcare providers in Southern California, effectively halting caries progression in early childhood caries cases. Nevertheless, SDF was not readily available in certain European countries and the USA.[14] In 2014, the US Food and Drug Administration approved SDF for managing tooth hypersensitivity.[17]
SDF's extensive use began in China in the early 21st century as a caries arresting agent in school-going children. A series of in-vitro studies highlighted SDF's anti-plaque potential due to its bactericidal action on Streptococcus mutans. Between 2005 and 2009, Australia conducted in-vitro studies confirming SDF's effectiveness against Streptococcus mutans and dental biofilm as a caries-arresting and antimicrobial agent.[18], [19] Similar studies were conducted in Nepal and the US, demonstrating SDF's efficacy as a caries arresting agent. In 2013, SDF was utilized to prevent root caries in the elderly.[20] Studies in India provided evidence of the successful use of SDF as a caries arresting agent. A 2018 study in the USA found that SDF effectively arrested active caries in the primary teeth of young children and was well-received by their parents.[21] Numerous ongoing studies in various countries aim to establish SDF as a valuable tool for dental public health professionals in addressing dental caries among at-risk populations.
Initially approved in the United States in 2014 to reduce dentinal hypersensitivity, Health Canada later approved it as an anti-caries product. SDF marketed as Advantage Arrest by Elevate Oral Care, received approval for sale in Canada in February 2017.[22] The U.S. Food and Drug Administration now recognizes SDF as a therapy for arresting tooth decay, with an official code (D1354) designating it as an interim caries arresting medicament.[23] Silver compounds have been employed in medicine and dentistry for over a century, and SDF represents a promising advancement in caries management.
What is it and How Does it Work?
SDF is a clear liquid product consisting of water, 25% silver, 5.5% fluoride, and 8% ammonia, resulting in a 38% SDF medicinal ingredient content.[24] While various SDF concentrations (10%, 12%, 30%, and 38%) are available, reviews recommend using a 38% concentration for preventing and arresting dental caries in children.[25] SDF is applied exclusively to carious lesions, both cavitated and non-cavitated, forming a protective layer on demineralized enamel and dentin. This layer enhances resistance to acid dissolution and enzymatic digestion of collagen, promoting mineralization and the formation of hydroxyapatite and fluorapatite. Silver and fluoride ions penetrate enamel (up to 50 µ) and dentin (up to 200 µ), stimulating remineralization and providing antimicrobial action, which is sustained over time.[26]
The antimicrobial action of SDF disrupts bacterial cell walls, leading to cellular distortions and loss of viability. Additionally, it inhibits bacterial enzyme activities and metabolic processes, ultimately causing microbial death. Studies have shown that 38% SDF enhances remineralization of initial carious lesions, outperforming 1000 ppm fluoride toothpaste alone.[27] SDF exhibits approximately 80% caries arrest, with improved results upon repeat applications, although a single application becomes less effective over time. It is recommended to apply SDF semi-annually, with some clinicians suggesting a one-month follow-up for assessment. Moreover, SDF applied to carious lesions appears to prevent new caries on other tooth surfaces, particularly in children.
SDF's preventive effect surpasses that of fluoride varnish, especially when accompanied by oral hygiene education. Its long-term application duration remains uncertain. In-vitro studies have demonstrated SDF's ability to increase biofilm pH, reduce dentin demineralization, and exhibit antimicrobial action against cariogenic bacteria.[28], [29] However, SDF-treated teeth may develop black stains due to silver phosphate precipitation.
The interaction of fluoride with tooth structure and silver's antimicrobial role are important considerations. Silver prevents disulfide bond formation in amino acids and nucleic acids, disrupting protein and nucleic acid structure and function, ultimately leading to bacterial cell death.
Mechanism of Action
A) Cariostatic Action: Another mechanism involves the cariostatic action of products resulting from the reaction between SDF and tooth minerals. SDF reacts with tooth mineral hydroxyapatite to release calcium fluoride (CaF2) and silver phosphate (Ag3PO4).[30] These products enhance the resistance of dentin to acid decalcification and inhibit the penetration of acid into deeper dentin layers. Fluoride ions in SDF also increase dentin's resistance to acid, further reducing acid penetration.[27] When applied in vivo, fluoride ions penetrate dentin to a depth of 50–100 μ.
B) Occlusion of Dentinal Tubules:[31] One mechanism involves the occlusion of dentinal tubules with silver. This occlusion prevents the invasion of caries through the dentin's main channels, the dentinal tubules. When SDF is applied to dentin, it reduces dye permeability and enhances electric resistance. Silver and its compounds from SDF block the diffusion of acid and the invasion of microorganisms into the dentinal tubules.
The basic chemical reaction is shown below:
Ca10(PO4)6(OH)2 + Ag(NH3)2 → CaF2 + Ag3PO4 + NH4OH CaF2 → Ca++ + 2F- Ca10(PO4)6(OH)2 + 2F− → Ca10(PO4)6F2 + 2OH−
The Ag3PO4 that is formed on the tooth is insoluble in acid attacks. The CaF2 formed as a reaction product becomes a pool of fluoride ions for the formation of fluorapatite (Ca10(PO4)6F2). It is also proved that fluoride ions enhance the calcification of tooth, restore lattice imperfection, and improve the crystallinity of HA.
Additionally, silver's oligodynamic action inhibits microbial growth. The obturation of dentinal tubules reduces the surface area vulnerable to caries attack and covers the peritubular zone, the most susceptible part of dentin to demineralization. These factors contribute to increased resistance against recurrent caries. Recent studies also suggest that 38% SDF inhibits demineralization and preserves collagen in demineralized dentin.
C) Anti-Enzymatic Actions: SDF's reaction products with the organic components of the tooth may contribute to its caries-arresting properties through anti-enzymatic actions. This antibacterial effect arises from the inhibition of enzyme activities and the prevention of dextran-induced agglutination of cariogenic strains of Streptococcus mutans. Dentin treated with Ag(NH3)2OH by ionophoresis showed increased resistance to trypsin, potentially due to the reaction of silver with dentin's organic components. This increased resistance to enzymatic degradation may inhibit caries development. SDF application on tooth surfaces has also been shown to increase dentin's resistance to trypsin, cathepsin, matrix metalloproteinase, and collagenase.[32], [33] These actions of SDF on tooth organics may further contribute to caries inhibition.
Clinical Recommendations
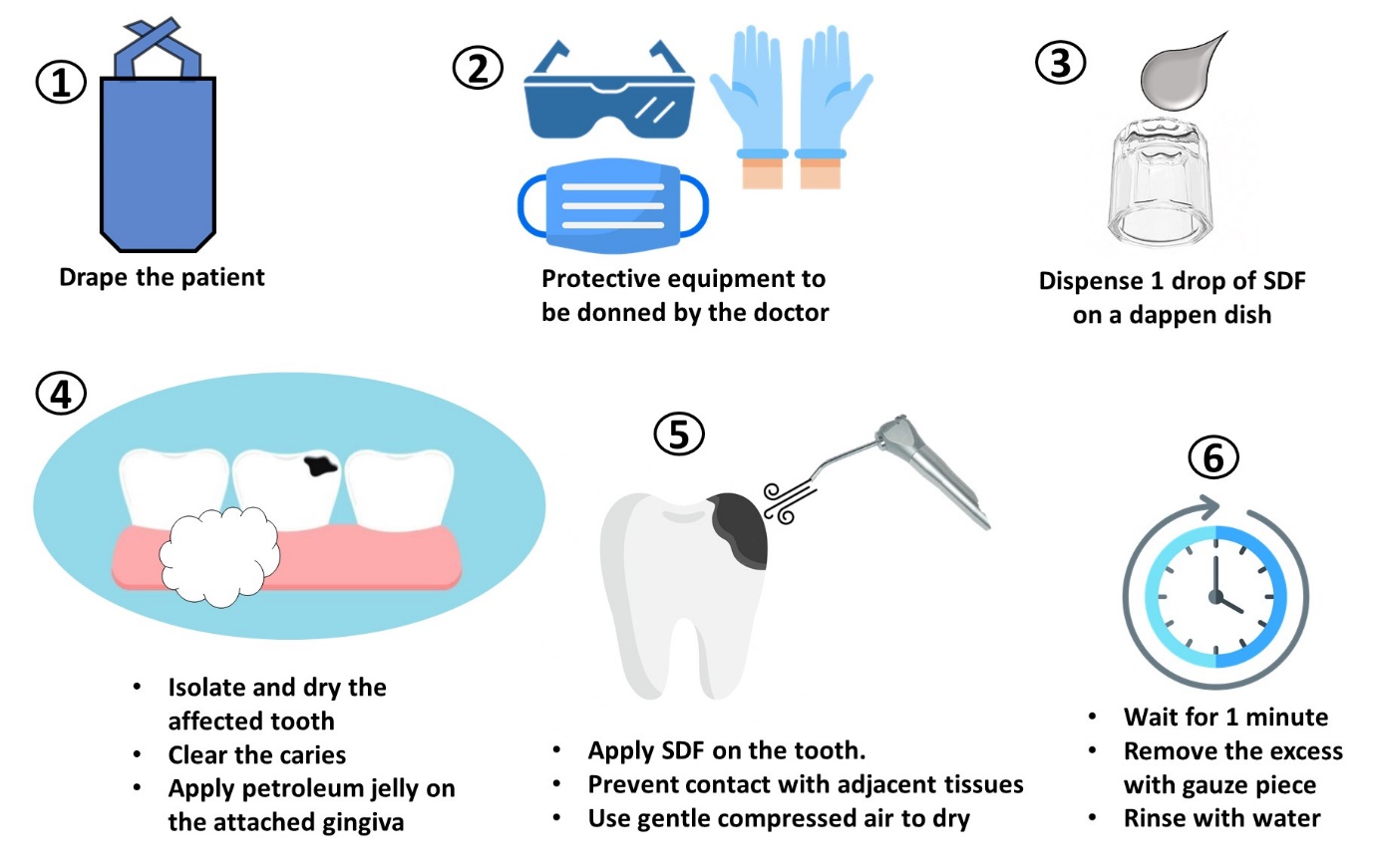
The procedure to apply SDF is depicted in [Figure 1]. It has been suggested that excavation of carious dentin before applying SDF may not always be necessary. It primarily addresses esthetic concerns and can be applied for 10 seconds to 3 minutes, with 1 minute being ideal, using gentle compressed air drying. After shorter applications, postoperative evaluation and potential reapplication are advised. Avoid eating or drinking for 30 minutes to 1 hour after SDF application. Regular 6-monthly application is advised. Informed consent and proper documentation are crucial due to potential adverse effects such as black staining. Regular follow-ups are recommended for long-term success based on individual risks.[23]
Utility of SDF
SDF is a versatile treatment option for caries management, offering benefits in various clinical scenarios, including difficult access cases, high caries risk patients, and prevention of pit and fissure caries.[34] The utility of SDF in dentistry, with an emphasis on pediatric dentistry, is described below and delineated pictorially in [Figure 2].
Preventing Early Childhood Caries (ECC): SDF application can arrest caries in young children, eliminating the need for invasive treatments that often face behavioral challenges. It prevents tooth loss, which can lead to psychological and phonation problems, and supports normal jaw bone growth and timely permanent tooth eruption.
Root Caries Prevention: Annual SDF application effectively arrests root caries, outperforming four times per year fluoride varnish in both children and elders.
Dentinal Hypersensitivity: SDF can treat dentinal hypersensitivity by occluding dentinal tubules, reducing sensitivity to mechanical and thermal sensations. Repeated application has been found effective.
Disinfecting Root Canals: SDF can serve as an endodontic irrigant by virtue of its potent antimicrobial properties, reducing microbial load within root canals.
Behavioral or Medical Management Issues: Since SDF is non-invasive and does not involve pain that is otherwise felt during dental treatment, it is more accepted by patients, particularly children. It further reduces the chances to develop dental fear commonly noted in children due to pain during treatment. In patients having conditions that contraindicate invasive treatment procedures, the non-invasive nature of SDF application enables intervention for the disease.
Preventing Secondary Caries: SDF enhances cavity wall resistance to recurrent caries and can be used as a preventive measure after restorative procedures.
Community Dental Health Programs: SDF offers advantages in developing countries, including pain and infection control, affordability, simplicity of application, minimal infrastructure requirements, and low infection risk.

SDF and Caries
SDF is effective for arresting caries lesions and preventing new caries in both primary and permanent teeth.[19], [20], [21] It can be applied twice yearly as a starting point and is a viable treatment option for high-risk, high-need patients. No caries excavation is necessary, but clean surfaces are desirable for direct contact. Study application times vary, but manufacturer-recommended times are consistent with the best results. Initial use on posterior teeth and large cavities might be considered, with tailored re-application as needed. Combining SDF and fluoride varnish is an open question, and alternating their use is a potential solution. Anterior teeth show higher rates of caries arrest. In clinical settings, curing light use after drying may improve arrest in posterior areas not exposed to natural light.
Advantages of SDF
The main advantages of SDF include pain and infection control at an affordable cost, simplicity of treatment, minimal infrastructure requirements, and a non-invasive procedure that minimizes infection risk. In clinical applications, SDF is valuable for managing patients with high caries prevalence, such as those with xerostomia or S-ECC.[35] It can arrest caries progression, allowing for comprehensive care at a later date. Studies have shown SDF's effectiveness in arresting cavitated and incipient carious lesions. It is particularly useful in patients with behavioral problems or medical limitations. SDF is effective for patients with limited access to dental care, especially those at high caries risk, medically challenged individuals, and emotionally challenged children.[36] SDF can also extend treatment plans, improving the quality of life for patients with prolonged care needs. Additionally, SDF can address caries problems in masses that don’t have access to dental clinics which is especially beneficial in low-income countries. Its antibacterial and caries-preventive properties make it useful in this context.
Safety Concerns about SDF
The average LD50 by oral administration is 520 mg/kg, and by subcutaneous administration is 380 mg/kg.[37] SDF is considered safe for use, even in children, with a significant safety margin. For example, a single drop on a 10 kg child provides a 400-fold safety margin. Preliminary studies suggest that serum concentrations of fluoride and silver after topical SDF application pose little toxicity risk when used in adults. The safety and efficacy of SDF have been extensively studied over the years which has revealed certain conclusions regarding its use.
SDF has a higher fluoride concentration than expected in some commercial products, raising concerns about toxicity. However, studies from different regions have shown favorable results with no severe adverse reactions or dental fluorosis when used appropriately. Pulpal responses to SDF application have generally been favorable, with no severe damage reported. There is no evidence to suggest that SDF causes severe reactions such as contact dermatitis or stomatitis. Recent short-term studies suggest little to no toxicity risk when used in adults.
Adverse Effects
The major disadvantage is the black discoloration of arrested carious lesions, particularly aesthetically unacceptable for anterior teeth.[38] It is important to note that SDF treatment causes permanent black staining of caries lesions, which may affect a patient's aesthetic concerns. Patients' quality of life and their priorities regarding physical appearance should be considered when assessing risks and benefits. This warrants informed consent and documentation before the SDF application although acceptance of staining may be higher than expected. SDF has potential adverse effects in large quantities, including nephrotoxicity or hepatotoxicity, intestinal irritation, and graying of the sclera.[39]
Common adverse effects include taste-induced nausea, pulpal irritation, and staining, with staining affecting not only teeth but also soft tissues, restoration margins, skin, clothing, and operatory surfaces.[40] For bonding procedures, rinsing may be recommended, but some studies suggest SDF doesn't affect the bonding of glass ionomers and composites. In long-term studies, adverse pulpal responses were minimal, and there were no reported deaths or systemic adverse effects when used as per the manufacturer's recommendations. Gingival responses have been minimal, and measures like coating nearby gingiva with petroleum jelly and using small micro-sponges help minimize contact.
SDF darkens carious lesions, and applying a saturated solution of potassium iodide may reduce staining.[38] Patients may experience a transient metallic or bitter taste. SDF may cause temporary skin "tattoos" but poses no harm and fades naturally. SDF can stain clinical surfaces and clothing, requiring immediate cleaning with water, ethanol, or bleach.
SDF does not affect bonding of composite to non-carious dentin using various bonding systems.[41] Rinsing with water after SDF application can prevent a decrease in bond strength for GIC. SDF may decrease the dentin bonding strength of resin-based crown cement, suggesting rinsing for direct restorations and removal of superficial dentin for crown cementation.
Concerns and Barriers
It may cause grayish-black or black staining, which should be noted in records to avoid misinterpretation as incipient caries.[38] Pits and fissures are more susceptible to caries due to their morphology, and topical fluoride applications are less effective in preventing them compared to smooth surfaces. Concerns include fluoride dose, tooth discoloration, and pulpal or gingival reactions. Parents' acceptance varies, but it tends to increase with barriers to conventional treatment.[42] The black staining following SDF application is due to silver phosphate formation. Potassium iodide (KI) may reduce staining, but its effectiveness needs further investigation.
A study involving parents found that, for posterior cases, 67.5% of parents tolerated the staining, with 53.6% preferring SDF treatment over traditional approaches.[42] For anterior applications, these percentages were lower. When given the choice between SDF and treatment under general anesthesia, a significant proportion of parents preferred SDF treatment.
SDF can be a valuable option for noncooperative, medically compromised patients, those awaiting operating room treatment, noncompliant individuals, and those with extensive caries. Informed written consent is crucial before the SDF application. Patients with a silver allergy, open lesions, stomatitis, or ulcerative gingivitis should avoid SDF treatment, as the staining can be permanent in subepithelial cases.
Contraindications to SDF include allergy to silver, pregnancy (especially during the first six months of breastfeeding), breastfeeding, ulcerative gingivitis, and stomatitis.[43] Pregnancy considerations for SDF therapy are currently limited, and the staining of epithelium typically resolves with epithelial turnover. SDF is a viable choice for patients seeking minimally invasive dentistry, not limited to specific categories of patients.
Nano Silver Fluoride (NSF)
NSF is an experimental formulation with silver nanoparticles, chitosan, and fluoride, offering preventive and antimicrobial properties without black staining. NSF is stable, safe, cost-effective, effective in arresting caries, and has the potential for broader application.[44] It is biocompatible and bactericidal, with low toxicity and a lack of metallic taste. The agent doesn't stain dental tissue black and is suitable for economically disadvantaged communities. NSF is a promising anti-caries agent and a potential alternative to SDF. Dietary controls and oral hygiene instructions are essential components of caries management in underprivileged communities. Both SDF and NSF are promising anti-caries agents with advantages and some concerns.[45] SDF has been extensively studied and used clinically, while NSF offers a potential alternative with the advantage of not staining dental tissue black. Further research and clinical trials are needed to assess their long-term safety and effectiveness.
Conclusion
In conclusion, Silver Diamine Fluoride has demonstrated antibacterial properties, remineralization capabilities, and potential benefits in caries control, particularly in young children. While black staining is a known side effect, the health advantages of preventing tooth decay, especially in areas with limited access to dental care, outweigh this concern. However, maintaining good plaque control remains essential for successful caries control. SDF has the potential to revolutionize pediatric and community dentistry due to its safety, efficiency, feasibility, and effectiveness in preventing and arresting dentine caries.
Source of Funding
None.
Conflict of Interest
None.
References
- S Anil, PS Anand. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr 2017. [Google Scholar] [Crossref]
- H Çolak, ÇT Dülgergil, M Dalli, MM Hamidi. Early childhood caries update: A review of causes, diagnoses, and treatments. J Nat Sci Biol Med 2013. [Google Scholar]
- D Duangthip, KJ Chen, SS Gao, ECM Lo, CH Chu. Managing early childhood caries with atraumatic restorative treatment and topical silver and fluoride agents. Int J Environ Res Public Health 2017. [Google Scholar]
- GZ Wright, A Kupietzky. . Behavior management in dentistry for children 2014. [Google Scholar]
- S Chenicheri, R Usha, R Ramachandran, V Thomas, A Wood. Insight into oral biofilm: primary, secondary and residual caries and phyto-challenged solutions. Open Dent J 2017. [Google Scholar]
- S Jones, BA Burt, PE Petersen, MA Lennon. The effective use of fluorides in public health. Bull World Health Organ 2005. [Google Scholar]
- AP Munevveroglu, O Ruhan. Comparison of Different Fluoride Solutions Application on Dentin Caries Lesions in Primary Teeth. Oral Health Dent Sci 2020. [Google Scholar]
- V Naegeli. Deut schr Schweiz Naturforsch Ges. 1893. [Google Scholar]
- S Ai, T Ishikawa, A Seino. Ohaguro" traditional tooth staining custom in Japan. Int Dent J 1965. [Google Scholar]
- EA Stebbins. What value has argenti nitras as a therapeutic agent in dentistry?. Int Dent J (Phila) 1891. [Google Scholar]
- PR Howe. A method of sterilizing and at the same time impregnating with a metal affected dentinal tissue. Dent Cosmos 1917. [Google Scholar]
- GG Craig, KR Powell, MH Cooper. Caries progression in primary molars: 24‐month results from a minimal treatment programme. Community Dent Oral Epidemiol 1981. [Google Scholar]
- S Mohanty, D Satyarup, R Nagarajappa, I Mahapatra, RP Dalai, S Sahu. Silver Diamine Fluoride: Game Changer in Dental Public Health: A Review. Indian J Forensic Med Toxicol 2020. [Google Scholar]
- AC Scully, JF Yepes, Q Tang, T Downey, G Maupome. Utilization of silver diamine fluoride by dentists in the United States: a dental claims review. Pediatr Dent 2020. [Google Scholar]
- P Sasikumar, H Nagarajan, Silver, FA Review. Silver diamine fluoride- A Review. Int J Community Dent 2022. [Google Scholar]
- SS Gao, G Amarquaye, P Arrow, K Bansal, R Bedi, G Campus. Global oral health policies and guidelines: using silver diamine fluoride for caries control. Front Oral Health 2021. [Google Scholar] [Crossref]
- YO Crystal, R Niederman. Evidence-based dentistry update on silver diamine fluoride. Dent Clin 2019. [Google Scholar]
- A Callaway, H Meisberger, B Willershausen, E Stender. 55th ORCA Congress. Caries Res 2008. [Google Scholar]
- CH Chu, ECM Lo. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent 2008. [Google Scholar]
- W Zhang, C Mcgrath, EC Lo, JY Li. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res 2013. [Google Scholar]
- J Clemens, J Gold, J Chaffin. Effect and acceptance of silver diamine fluoride treatment on dental caries in primary teeth. J Public Health Dent 2018. [Google Scholar]
- . Advantage Arrest Silver Diamine Fluoride 38%. . [Google Scholar]
- DA Young, RL Quock, J Horst, R Kaur, JK Maclean, JC Frachella. Clinical instructions for using silver diamine fluoride (SDF) in dental caries management. Compend Contin Educ Dent 2021. [Google Scholar]
- FM Zheng, IG Yan, D Duangthip, SS Gao, EC Lo, CH Chu. Silver diamine fluoride therapy for dental care. Jpn Dent Sci Rev 2022. [Google Scholar]
- ZO Tolba, HS Hamza, DM Moheb, HE Hassanein, HM ElSayed. Effectiveness of two concentrations 12% versus 38% of silver diamine fluoride in arresting cavitated dentin caries among children: a systematic review. Egypt Pediatr Assoc Gaz 2019. [Google Scholar]
- J Manuschai, S Talungchit, S Naorungroj. Penetration of Silver Diamine Fluoride in Deep Carious Lesions of Human Permanent Teeth: An In Vitro Study. Int J Dent 2021. [Google Scholar] [Crossref]
- K Punyanirun, T Yospiboonwong, T Kunapinun, P Thanyasrisung, C Trairatvorakul. Silver diamine fluoride remineralized artificial incipient caries in permanent teeth after bacterial pH-cycling in-vitro. J Dent 2018. [Google Scholar]
- ML Mei, Z Yan, D Duangthip, JY Niu, OY Yu, M You. Effect of silver diamine fluoride on plaque microbiome in children. J Dent 2020. [Google Scholar]
- BY Liu, J Liu, D Zhang, ZL Yang, YP Feng, M Wang. Effect of silver diammine fluoride on micro-ecology of plaque from extensive caries of deciduous teeth-in vitro study. BMC Oral Health 2020. [Google Scholar] [Crossref]
- ML Mei, EC Lo, CH Chu. Arresting dentine caries with silver diamine fluoride: what’s behind it?. J Dent Res 2018. [Google Scholar]
- A Kiesow, M Menzel, F Lippert, JM Tanzer, P Milgrom. Dentin tubule occlusion by a 38% silver diamine fluoride gel: an in vitro investigation. BDJ Open 2022. [Google Scholar]
- ML Mei, QL Li, CH Chu, CK Yiu, EC Lo. The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater 2012. [Google Scholar]
- ML Mei, L Ito, Y Cao, QL Li, CH Chu, EC Lo. The inhibitory effects of silver diamine fluorides on cysteine cathepsins. J Dent 2014. [Google Scholar]
- S Nuvvula, SK Mallineni. Silver diamine fluoride in pediatric dentistry. J South Asian Assoc Pediatr Dent 2019. [Google Scholar]
- A Bakhtiary, S Taheri. Effectiveness of Silver Diamine Fluoride compared with Sodium Fluoride Varnish on Oral Saliva pH in the Children with Sever-Early Childhood Caries (S-ECC). J Res Appl Basic Med Sci 2022. [Google Scholar]
- G Molina, M Zar, A Dougall, C Mcgrath. Management of dental caries lesions in patients with disabilities: Update of a systematic review. Front Oral Health 2022. [Google Scholar] [Crossref]
- J A Horst, H Ellenikiotis, P M Milgrom. UCSF Silver Caries Arrest Committee. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc 2016. [Google Scholar]
- MM Aly, YM Yousry. Potential discolouration of silver diamine fluoride versus silver diamine fluoride/potassium iodide in primary teeth: a randomised clinical study. Br Dent J 2022. [Google Scholar]
- YO Crystal, R Niederman. Evidence-based dentistry update on silver diamine fluoride. Dent Clin 2019. [Google Scholar]
- D Duangthip, MH Fung, MC Wong, CH Chu, EC Lo. Adverse effects of silver diamine fluoride treatment among preschool children. J Dent Res 2018. [Google Scholar]
- M Firouzmandi, M Mohaghegh, M Jafarpisheh. Effect of silver diamine fluoride on the bond durability of normal and carious dentin. J Clin Exp Dent 2020. [Google Scholar]
- H Sabbagh, M Othman, L Khogeer, H Al-Harbi, AAY Abdulgader. Parental acceptance of silver Diamine fluoride application on primary dentition: a systematic review and meta-analysis. BMC Oral Health 2020. [Google Scholar]
- JW Farmer, S Singhal, L Dempster, C Quiñonez. Effectiveness, safety, and acceptance of silver diamine fluoride therapy and its implications for dental hygiene practice: Position paper and statement from the Canadian Dental Hygienists Association. Can J Dent Hyg 2018. [Google Scholar]
- S Tirupathi, SV Nirmala, S Rajasekhar, S Nuvvula. Comparative cariostatic efficacy of a novel Nano-silver fluoride varnish with 38% silver diamine fluoride varnish a double-blind randomized clinical trial. J Clin Exp Dent 2019. [Google Scholar]
- N Ammar, MM El-Tekeya, S Essa, MM Essawy, DM Talaat. Antibacterial effect and impact on caries activity of nanosilver fluoride and silver diamine fluoride in dentin caries of primary teeth: a randomized controlled clinical trial. BMC Oral Health 2022. [Google Scholar]
How to Cite This Article
Vancouver
Padawe D, Jagtap V, Takate V, Dighe K, Rathi G, Wankhade A. Silver diamine fluoride – ‘The silver bullet’ in pediatric dentistry: An overview of past, present and prospects [Internet]. Int Dent J Stud Res. 2023 [cited 2025 Sep 12];11(4):146-153. Available from: https://doi.org/10.18231/j.idjsr.2023.032
APA
Padawe, D., Jagtap, V., Takate, V., Dighe, K., Rathi, G., Wankhade, A. (2023). Silver diamine fluoride – ‘The silver bullet’ in pediatric dentistry: An overview of past, present and prospects. Int Dent J Stud Res, 11(4), 146-153. https://doi.org/10.18231/j.idjsr.2023.032
MLA
Padawe, Dimple, Jagtap, Vijaya, Takate, Vilas, Dighe, Kishor, Rathi, Gauri, Wankhade, Ajinkya. "Silver diamine fluoride – ‘The silver bullet’ in pediatric dentistry: An overview of past, present and prospects." Int Dent J Stud Res, vol. 11, no. 4, 2023, pp. 146-153. https://doi.org/10.18231/j.idjsr.2023.032
Chicago
Padawe, D., Jagtap, V., Takate, V., Dighe, K., Rathi, G., Wankhade, A.. "Silver diamine fluoride – ‘The silver bullet’ in pediatric dentistry: An overview of past, present and prospects." Int Dent J Stud Res 11, no. 4 (2023): 146-153. https://doi.org/10.18231/j.idjsr.2023.032
