Introduction
In ancient times, treatment for missing teeth relied on Removable partial dentures or fixed partial dentures. However, the field of dentistry underwent a transformative shift with the advent of dental implants. Despite challenges and complications, dental implants have emerged as a preferred treatment choice. These implants are prosthetic devices made of alloplastic material, placed within oral tissues or bones to support fixed or removable dental prostheses. While placing dental implants in the esthetic zone is highly desired, the quality of the bone remains a crucial factor in determining their positioning.
Dental implants are contraindicated in various comorbidities including myocardial infarction, epilepsy, endocarditis, history of osteoradionecrosis, smoking, and diabetes. Absolute contraindications encompass conditions like cerebrovascular accidents, bleeding history, heart transplant, immune suppression, active malignancy treatment, drug abuse, and psychiatric illness. Early complications like bleeding, infection, and pain can lead to implant failure. Factors influencing dental implant survival include age, implant length and diameter, bone quality, and implant location.
The anterior maxillary region poses challenges due to vital structures like the maxillary sinus and mandibular canals, often necessitating extensive augmentation procedures that are cost-intensive and time-consuming. Even with these efforts, success rates remain low, and risk of morbidity is higher. In cases lacking vertical height and cost-effectiveness concerns, basal implants are favored. Basal Osseo Integrated (BOI) and Basal Cortical Screw (BCS) implants, designed to utilize stronger basal bone, offer enhanced support and infection resistance. Screwable basal implants allow immediate fixation without incisions, reducing invasiveness and bone space requirements, thereby lowering peri-implantitis risk. This technique presents advantages over conventional implants due to immediate loading.1, 2, 3, 4, 5, 6
A case study is presented involving a female patient with diabetes who lost a tooth due to trauma. The basal implant technique was employed, accompanied by a fixed prosthetic to restore her oral function. The study also provides a succinct overview of pertinent previous research.
Case Study
A 37 years old female in normal gait visited, ‘Department of Prosthodontic’ with Chief complain missing tooth in the upper anterior region. On intra oral examination, it was found to be fracture that falls in Ellis class 4 fracture (1970) and 5.03.52 Classification of WHO (1978) with respect to Maxillary Central Incisor{11}, were as, Maxillary lateral incisor{12}, Maxillary central and lateral incisor of second Quadrant {21, 22} fall in Ellis class 5.7 On further, enquiries about history of present illness, The patient revealed Trauma (Due to fall) three years back and remains asymptomatic till date. Primary concern of visit was aesthetic reason. Medical history disclosed recently developed Diabetes Mellitus type 2, and on oral medication. (Metformin 500 mg BD) since 2 years. Despite of the fact that she is diabetics and did not seek any professional dental help, her periodontal conditions was not comprised. No any other Periodontal problem and oral lesion was recorded.
Acknowledging, patients medical condition various prosthetic options including Removal Partial denture after extracting of remaining Non-vial tooth/root structure, Fixed partial denture excluding Implant, Basal Implant supported fixed partial denture. The patient wishes to have any procedure that is less traumatic, in fewer sitting and fixed option. Thus, After through evaluation we opted to replace missing teeth with Basal implant supported Fixed partial denture. And even preoperative radiograph suggested sound bone and sufficient space for placement of a long implant with bicortical engagement.
The patient was send for routine blood investigation required for implant along with HBA1C to evaluate Diabetic conditions. As, a matter of fact that in case of uncontrolled Diabetes probability and possibility of implant failure is high. (DM) and blood results was found to be within normal limits, in case of HBA1C was 6.5% indicating Controlled diabetes.
Prior to the surgery oral prophylaxis was done patient was asked to risen oral cavity with chlorhexidine 0.2% for 2 minutes. Local anaesthesia, lidocaine 2% with epinephrine (epinephrine 1:100,000 (0.01 mg/mL) was used to innervate infraorbital nerve and nasopalatine nerve for desirable effect. Flaps were raised for the extraction of residual root structure in maxillary right central incisors. After extraction curettage was done followed by copious irrigation with povidone-iodine.
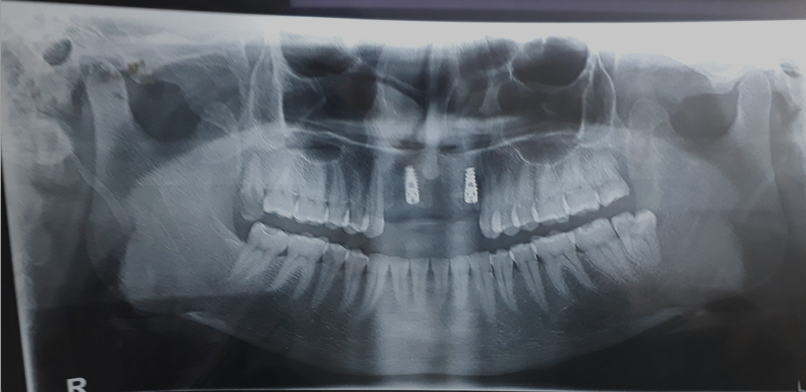
The use of single piece immediate implant (BSC) in the newly extracted area provide better attachment for a basal implant. A flapless immediate implant procedure was used for placing implants. Considering the demands and needs of the patients, It was decided to place a 3.5 mm diameter and 21 mm insertion-length Bicortical screw implant in the edentulous space of maxillary right central and left lateral incisor.(Figure 1)
To avoid secondary infection or complications in the placement site or implant. The strict protocol of sterilization before and during the producer was followed. Access to the external compact bone was achieved using a slow speed bur, 3.5mm diameter bur, with constant cooling. This is done to avoid overheating of the osteomy site (39).
Once, tactile contact with the opposite cortical bone was felt, bur was immediately stopped. Considering the coarse nature of the cancellous bone, further drilling is not needed for implant placement of diameter 3.75 mm. Ostomy with 3.5mm drill is usually sufficient to screw a soft tapping 3.75mm implant.8
Primary stability of implant was determined by Surgeon perception along with RFA (Resonance Frequency Analysis), tactile feeling, torque test, and percussion test. And at 35 N of torque primary stability was established.
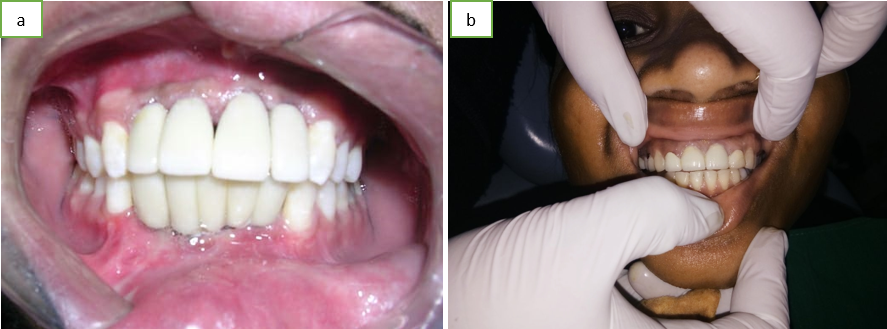
Metal cutting bur was used for milling the abutment to achieve optimal position and it’s adjustment. Then the flap was covered and sutured. Immediate loading of the implanted area with temporary crown was done.(Figure 2, Figure 3)
Figure 1
Showing flapless technique was used for accessing the basal bone and Bicortical implant placement. 3.5 mm diameter and 21 mm insertion-length Bicortical screw implant in the edentulous space of maxillary right central and left lateral incisor.

Figure 2
Raised flap was sutured. Thought, flapless technique was used for implant placement. Flaps were raised for the extraction of residual root structure in maxillary right central incisors.

Figure 3
Image showing position of implanted bicortical screw prior to permanent prosthetic. Slightly bleeding is seen as temporary prosthetic was removed. Wound is healed properly.

Impression of maxillary and mandibular ach was recorded using addition silicon impression material and was then transferred to master cast. Further, it was send to dental lab for the preparation of Fixed bridge and ceramic prosthesis. Patient was asked to visit after 10 days for permanent crown and bridge prosthesis. Moreover, Subject was kept in antibiotics therapy with analgesic For 10 days. (Amoxicillin 500mg + clavulanic acid 125 mg BD, Metronidazole 400 mg BD and Aceclofenac 100mg + Paracetamol 325mg + Serratiopeptidase 15mg BD). On 10th day areas was completely healed and OPG radiographs show no abnormalities Or anything periodontal disease or complications due to implant placement. Hence, patient was ready for final fixed prosthesis.Figure 5
Permanent prosthetic was delivered on day 10 post operative and was kept on follow up for 12 months.(Figure 4)
Discussion
The maxillary and mandibular jaw bone comprise of two parts, alveolus or crestal that contain tooth and the basal bone. As, alveolar bone/crestal bone is less dense in nature, this are exposed and subject to wide range of infection from oral cavity, tooth borne pathology, inquires or iatrogenic factors. Hence, high rate of infection and absorption is observed. In other hand, basal bone are much deeper and denser (I.e. heavily corticated) thereby, less prone to infection and reabsorption. This dense nature of basal bone provide excellent support and stability to implant. 9, 10, 11, 12 It is postulated that any dental implants material when placed in basal bone. This surgical procedures/process triggers the cascade responsible for bone healing. Thus interlocking of bone and implant body occur and later, biological fixation through continues bone apposition and Remoulding towards the implant. 13 Healing process is also time dependent and clinically asymptomatic ridge fixation of alloplastic material is achieved. 14, 15 Primary implant stability did not depend on total bone thickness but tended to increase with either increasing bone mineral density or overall cortical bone thickness. 14, 15
Retrospective review of various literature indicated that survival rate is 99% of dental implants that followed bicortical smooth surface implant concept with immediate loading in patients with or without periodontal conditions. 16 It has been observed that cumulative survival at 12, 24, and 35 months for I implants healed socket was around 98.6%, 97.9%, and 97.9% respectively. Were as, in fresh extracted socked survival rate was around 99.6%, 99.0%, and 99.0%. 16 Interestingly, various published literature supported this argument that fresh wound or recently extracted socked has higher survival rate as compared to previously healed socket and found result to be similar. 17, 18, 19, 20, 21, 22 Immediate implant just after extraction in fresh wound helps in maintenance of vertical dimension, elimination of reline procedures and interim denture therapy, and potential improvement of soft tissue healing hence, additional advantage and this could also be beneficial in rehabilitation of complete edentulous patients with appropriate restorative and surgical techniques. 23 Even in case of edentulous maxilla authors has suggest, 4 to 6 implant is sufficient in rehabilitation of mouth supported by Fixed prosthetic. 24 Anterior maxilla implant are more stable and less venerable to failure as compared to posterior implant. In a 5 five years retrospective study authors conclude that parafunctional habits also add in dental implants failure by loosing of screw, fracture of implant screw and porcelain. It was also postulated that High occlusion load should be considered as risk factors.
As Bicortical implants are an excellent alternative to traditional two-stage implant systems which require ideal bone conditions and time for osseointegration. In our case we also opted the same technique i.e. BSC with immediate loading. Knowing the fact that patients is Diabetic and after considering patients requirements conventional implant was opted out. Published literature has also suggest that even in case recent myocardial infarction, cerebrovascular accident, immunosuppressant therapy, chemo and/or radiotherapy and bisphosphonate therapy Basal implant can be done. 11, 12
Diabetes Mellitus is a condition in which beta cell of pancreas is not able to produce sufficient amount of insulin or even the amount of insulin released from beta cell become resistance to it’s receptor which leads to chronic disorder of carbohydrate metabolism along with Lipids and protein metabolism. 25 As a result distortion in physiological equilibrium of glucose utilization by tissue occur. Additional to this alterations in liberation of glucose by liver and production-liberation of pancreatic anterior pituitary and adrenocortical hormone is also seen. 25 Evidence has suggest that constant increase glucose levels in diabetic patients tends to decrease collagen production during callus formation. Also altering the activities of parathyroid hormones responsible for Ca and P metabolism. Hyperglycaemia inhibit osteobalsic activity and increase osteoclastic activities also induce apoptosis of bone cells because of presence of inflammatory meditators. It also induce degrading effect on bone matrix formation, diminish growth and accumulation of extracellular matrix. Thus, as a consequence of this alternation, it hamper the bone formation during healing. Numerous authors have suggest the same in their literature. In case of basal implant, diabetic conditions is not a huge concerns, provided that diabetic is in controlled. 11 Evidence has suggested that if diabetic is in control, there is no significant difference in survival rate of dental implants. Even in case of old diabetic patients 100% survival rate has been achieved. 11 Although, some of the studies reported lower survival rate in older patients but no significant co-relation was established with diabetic conditions.
In our study we also, had similar findings, Patient was kept in follow up for 12 month and No any significant mal formation of bone was observed. Stability was maintained without any complain of loosening of implant or any post operative complications. Although, our study is limited to one patient case study but the fact that bicortical implant with immediate loading has higher survival rate and even comorbidities like diabetic conditions.
Conclusions
Based on the present study we found no further complication has arisen even after follow up for a year due to basal implant or diabetic history. In case of diabetic patients, basal dental implants may be considered as a treatment options, after evaluation of various factors like controlled diabetic, cost, time and aesthetic preference of patients. The unquestionable advantage or benefits of bicortical implant uses are because it significantly reduces number of visit and cost-effective.
However, the professional handling this procedure should be highly skilled as this technique is considered as highly sensitive and require proper execution. This approach is relatively new and being widely practised by leading dentist in India, professional should come out of their comfort zone of in popularising this technique.
Although, limited evidence and articles are available in medical data base determining its efficiency and success rate of bicortical basal implant in diabetic patients, and our case study is based on single patient, yet, this technique may be considered as safe for patients with controlled diabetic profile, though, further studies and controlled clinical trials are always mandated to determine its efficiency, success rate and safely of this technique in rehabilitation of full or partial mouth in diabetic patients.