Introduction
The mutans strain of Streptococcus microbes, responsible for cavities in teeth, is combated by the caries vaccine by strengthening the immune system's potency. When a vaccine is injected into the bloodstream, the body responds by producing antibody that target the bacteria, halting their ability to multiply and dissemination. The vaccine also targets the bacteria's biofilm-forming ability, making it difficult for them to stick to the teeth and cause cavities. The caries vaccine presents several benefits, including reduced probability of dental caries, cost-effectiveness, and low risk of side effects. It has the potential to revolutionize oral healthcare worldwide by offering a long-term, practical solution to dental caries.1, 2, 3
Dental Caries Eepidemiology
The investigation of the prevalence, incidence, and causes of ailments and other health issues in communities are known as epidemiological studies. Tooth decay is one of the many common persistent and transmissible illnesses impacting people globally, so knowing its prevalence is crucial to figuring out how it spreads and what variables increase the chance of developing it.
Every generation is affected by dental caries, albeit younger ones are more frequently affected. Around the world, the disease impacts between 60 and 90% of youngsters and about one hundred percent of grownups. The disease is more prevalent in low-income and disadvantaged populations and is associated with poor oral health and hygiene practices. Dental caries prevalence varies significantly depending on geographical locations, lifestyle, dietary practices, socioeconomic status, and oral hygiene habits. 4, 5
Risk factors that contribute to dental caries development include consumption of sugary foods and drinks, poor oral hygiene, lack of fluoride exposure, and decreased saliva production. Furthermore, some medical conditions and medications also increase the risk of developing dental caries, such as radiation therapy, cervical chemotherapy, type 2 diabetes, a condition called Sjogren's syndrome, etc.
Understanding the epidemiology of dental caries is essential in designing public health programs aimed at reducing the prevalence of the disease. Preventive measures such as regular dental check-ups, brushing with fluoride toothpaste, and avoiding excessive sugar consumption are vital in lowering the prevalence of tooth decay in the community. 6, 7
Microorganisms and Dental Caries
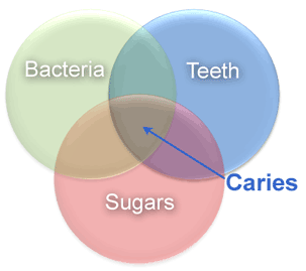
Due to its propensity for flourishing in the presence of dietary carbohydrates, especially sucrose, Streptococcus mutans is a significant cause of dental caries. It creates dental plaque, which is a type of sticky biofilm that makes it possible for bacteria to adhere to tooth surfaces. They break down carbohydrates inside these biofilms and generate acids as waste products, which erode tooth enamel and cause cavities. The development of caries is linked to Lactobacillus species, especially Lactobacillus acidophilus and Lactobacillus casei. They can colonise parts of the tooth that have previously been demineralized and flourish in acidic environments. This colonisation accelerates the deterioration. Caries, also sometimes referred to as decay of the tooth, is a prevalent oral condition brought on through the acid-producing microorganisms in the plaque on teeth demineralizing enamel as well as dentine. The mutans strain of Streptococcus and the genera Lactobacillus are among the most often found bacteria linked to tooth cavities. 8
These microorganisms break down sugars to create acidic compounds that can erode the protective coating on teeth and cause caries. S. mutans and other oral bacteria use a procedure known as fermenting to change the sugars in foods that are ingested into acid called lactic acid. The enamel as well as the dentin layers of the tooth may then be eroded by the acid that these microorganisms generate. Dental caries can also be caused by other things, like having bad oral habits, eating a lot of sweets and carbohydrates, and not using toothbrush or drinking water that contains fluoride. However, the occurrence of tooth decay is significantly influenced by the presence of micro organisms that produce acid. 9
In order avoid cavities from developing, one must reduce the percentage of microorganisms in their mouths, practice proper oral hygiene, and consume fewer sugary foods. Proper toothpaste application, frequent brushing and flossing and the use of rinsing by mouthwashes can help get rid of oral germs and lower the chance of getting cavities. Dental caries can also be avoided by eating a balanced diet with little sweets and carbohydrates. Sealants for dentistry and treatments containing fluoride can also aid in preventing decay from happening. 10, 11
Association Between Streptococcus Mutans and Dental Caries
A particular kind of organism called Streptococcus mutans(Figure 2) is frequently present in dental calculus and is closely linked to the emergence of cavities in the mouth, also known as dental rotting.
A type of gram-positive bacteria called S. mutans has the ability to produce lactate from carbohydrates in the diet, which can reduce tooth enamel and cause caries. Additionally, S. mutans has the capacity to manufacture glucans, which are clingy sugars that enable microbes to stick to the surfaces of teeth and create bio films. that shield them from scraping and hosts immunological reactions. 12, 13
S. mutans is highly adapted to the oral environment, as it is able to thrive in the low pH conditions of the mouth and can tolerate the antimicrobial compounds found in saliva. It can also co-aggregate with other oral bacteria to form complex microbial communities that contribute to dental plaque formation. One of the most effective methods in avoiding decay in the teeth is to stop S. mutans from growing and to lessen its capacity to generate acids and create biofilms. These range of strategies can be used to do this, including consistently practising good dental habits like flossing and cleaning your teeth, limiting dietary sugars and carbohydrates, and using fluoride-containing dental products such as toothpastes and mouthwashes. To prevent the formation of bacteria called S. mutans and shield tooth from deterioration, dental practitioners may also employ antimicrobial substances or pit and fissure sealants. 14
The Molecular Basis for Tooth Decay
The complicated interaction between microorganisms host-related factors, and external factors plays a role in the molecular predilection of tooth decay. The mutans strains of Streptococcus and particular kinds of Lactobacillus are the main genera of bacteria responsible for the emergence of cavities in the teeth. 15
As a consequence of breaking down food sugars, such microbes create acids, which can destroy tooth enamel as well as dentin and cause caries. S. mutans also makes glucans, which the microbes use to cling to the surfaces of teeth and create the biofilms that shield them from human immunological reactions and manual eradication. 16, 17
The development of tooth decay is significantly influenced by host variables as well. In addition to the form and makeup of the tooth enamel and dentin, genes may also affect pH levels and nature of the microbes that live in the mouth. Similar host variables found in saliva can have an impact on the development and physiology of oral microbes. 18, 19
Caries of the teeth can also be influenced by circumstances like eating habits and fluoride intake. While eating food rich in sugars as well as carbohydrates serves as a foundation for microbial growth and the generation of acid, fluoride aids in the remineralization of enamel on teeth and prevents the development of microorganisms that produce acidity. 20, 21
History of The Caries Vaccine
Caries vaccination, also known as anti-caries immunization, is a proposed method of preventing dental caries by using vaccines to stimulate the production of antibodies that target the bacteria responsible for tooth decay. 22
The idea of using vaccination to prevent dental caries dates back to the 1920s, when researchers first discovered that immunization with killed cultures of Streptococcus mutans could decrease the prevalence of cavities in the teeth in study experiments of animals.However, early attempts at caries vaccination in humans were largely unsuccessful, as the vaccines were not effective at inducing a strong immune response or protecting against natural infection. 23
In the 1970s and 1980s, researchers developed new approaches to caries vaccination, involving the application of a strain of S. mutans live isolated cultures along with the use of recombinant DNA technology to produce antigens that could stimulate an immune response. These new vaccines showed more promising results in animal studies and early clinical trials, but for an assessment of how well they work in humans, additional investigation is still required. 24
At present, the use of cavities vaccine as a means of avoiding cavities in the mouth has never been very common. However, investigation particularly in this area continues, and there is ongoing interest in developing new vaccines and immunization strategies to target the bacteria responsible for tooth decay. Other preventive measures, the primary components of preventive dentistry continue to be things like fluoride therapies, changes to ones eating patterns, and proper brushing and flossing habits. 25, 26
Caries Vaccination
Anti-caries vaccination, also known as caries vaccination, is a proposed method of preventing dental caries or tooth decay by using vaccines to stimulate the production of antibodies that target the bacteria responsible for tooth decay, primarily Streptococcus mutans. 27, 28
For the purpose of avoiding of tooth decay, many vaccinations, including whole-cell vaccinations, have been produced which are made from killed S. mutans bacteria, subunit vaccines that target specific antigens on the bacterial surface, and DNA vaccines that use genetically engineered plasmids to stimulate an immune response. 29
The development of anti-caries vaccines has been hampered by several challenges, including the need to identify antigens that are both immunogenic and specific to S. mutans, as well as the difficulty of inducing a strong and long-lasting immune response against the bacteria in the oral environment.
While some clinical trials of caries vaccines have shown promising results in reducing the incidence of caries, further studies are required to determine the reliability and security of these vaccines in bigger groups and over more extended spans for an extended period in order to prevent tooth decay in communities at greatest risk.
Currently, anti-caries vaccination is not widely used as a technique for stopping cavities in the mouth. However, findings in this area continues, and there is ongoing interest in developing new vaccines and immunization strategies to target the bacteria responsible for tooth decay. The mainstays of preventive dentistry continue to be things like fluoride therapy, dietary changes, and excellent brushing and flossing habits. 30, 31
Inactive Defence Through Cavities in the Teeth
Passive immunity against dental caries refers to the transfer of pre-formed antibodies to an individual, rather than stimulating their own immune system to produce the antibodies. This approach has been proposed as a potential method of preventing dental caries in those that are more susceptible to developing the disease, such as young children or those with compromised immune systems. 32
Passive immunity against dental caries can be achieved through the use of dental caries-specific immunoglobulin G (IgG) antibodies, which can be administered in various forms, including toothpastes, mouthwashes, and lozenges. These antibodies work by targeting the bacteria responsible for tooth decay, primarily Streptococcus mutans, and preventing them from adhering to tooth surfaces and producing acid. 33, 34
Several studies have investigated the effectiveness of passive immunity against dental caries, with mixed results. While some studies have shown a decrease in the prevalence of dental cavities in those who obtained dental caries-specific IgG antibodies, other studies have not found significant benefits. 35
One challenge with passive immunity against dental caries is the need for frequent and long-term administration of the antibodies, as the protective effects of the antibodies may diminish over time. 36, 37 Additionally, there may be safety concerns with long-term use of high levels of antibodies.
Overall, while passive immunity against dental caries remains an area of active research, it is not currently a widely used method of preventing dental caries. Other preventive measures, such as good oral hygiene practices, dietary modifications, and fluoride treatments, remain the mainstay of caries prevention. 38
Association with Cardiovascular System
There have been concerns about the potential for cross-reactivity between Streptococcus mutans, the bacteria targeted by caries vaccination, and human cardiac tissue. This is because S. mutans has been shown to share some similar surface antigens with human cardiac tissue, particularly with the protein myosin. 34
However, studies have shown that the S. mutans's degree of interaction against human cardiac tissue is relatively low and does not pose a significant risk. In fact, S. mutans's degree of interaction against human cardiac tissue is similar to that of other common bacteria, such as Streptococcus pneumoniae, which are not typically associated with cardiac disease. 38
Furthermore, the development of caries vaccines has taken these concerns into account, and efforts have been made to identify S. mutans antigens that are not cross-reactive with human tissues. In addition, clinical trials of caries vaccines have not reported any significant adverse effects related to interaction with cardiac cells from humans. 35
Overall, despite the possibility of S. mutans bacteria and cardiac tissue from humans being cross-reactive has been a concern in the development of caries vaccines, the level of cross-reactivity is relatively low and does not pose a significant risk. The safety and efficacy of caries vaccines are continually being evaluated in clinical trials, and efforts are being made to develop vaccines with high specificity and low risk of adverse effects.36
Opportunities for Immunization Against Caries
Caries vaccination, which involves the use of vaccines to prevent dental caries, throughout the past couple of decades, has served as the focus of substantial development and growth. While there is still much to learn about the potential benefits and risks of caries vaccination, there are several promising prospects that suggest that in this approach potential cavities in the teeth may be effectively avoided with this method.
Firstly, caries vaccination has the potential to provide long-lasting protection against dental caries. Unlike other preventive measures, such as fluoride treatments or good oral hygiene practices, which require ongoing maintenance and monitoring, vaccines provide a single dose of protection that can last for years or even a lifetime.
Second, immunization against cavities has been shown to reduce the risk of tooth decay in those at greatest risk including newborns and those with immune systems that are weak. This may facilitate a decrease in the prevalence of tooth decay in these groups, which can lead to significant pain, infection, and other health complications. 39
Thirdly, caries vaccination may be a cost-effective way to prevent dental caries. While the initial costs of developing and administering vaccines may be high, the long-term savings from preventing dental caries and associated health complications could be significant.
Despite having the potential to stop tooth decay, the caries vaccine faces obstacles and restrictions. These include the necessity for ongoing research of the safety and efficacy of vaccines, the potential for side effects, and the demand for long-term vaccination to maintain immunity. To completely comprehend the potential advantages and hazards of caries vaccines, more research and evaluation are required.
Conclusion
In the end, the creation of a cavities vaccine offers hope for both the cure and the avoidance of dental caries, an oral condition that is quite common in the globe. The intricacy of the oral microbiota and the requirement for long-term effectiveness and safety evidence remain obstacles despite the fact that a variety of ways have been examined for the creation of a caries vaccine. Preliminary findings from ongoing clinical studies of many vaccine candidates suggest that they could be successful in lowering the frequency and seriousness of dental caries. Additionally, a vaccination may offer even more defence from caries when combined with other preventative measures, such as the use of fluoride and excellent oral hygiene habits. A big step forward for dentists and the general population would be the creation of a caries vaccine, which has the potential to lessen the cost of cavities to people and hospitals worldwide.