Introduction
Peripheral Ossifying Fibroma is also known as Ossifying Fibroid Epulis, Peripheral Fibroma With Calcification, Calcifying Fibroblastic Granuloma. It is relatively common gingival overgrowth and reactive in nature rather than neoplastic.1 There are some other localized reactive lesions reported on the gingiva, like focal fibrous hyperplasia, pyogenic granuloma, peripheral giant cell granuloma (PGCG), and peripheral ossifying fibroma (POF). These lesions may arise as a result of irritants such as trauma, microorganisms, plaque, calculus, restorations, and dental appliance.2, 3 Shepherd et al. in 1844 made first description of this pathology as an alveolar exocytosis, and the term Peripheral Ossifying Fibroma(POF) was coined by Eversol and Robin in 1972.4 POF represents 2 – 9 % of all gingival epulis lesions5, 6, 7, 8, 9 and it is the third most common lesion of all localized reactive hyperplastic lesions after pyogenic granuloma and giant cell central granuloma,10 The prevalance of POFs are usually seen in childhood and younger ages, generally second decade of life. There is a slight female predilection and affecting maxilla (60%) more than mandible and generally found anterior canine and incisor region(50%).4 It is usually localized, rarely generalized. The typical appearance of POF is small gingival growth (Epulis) initially which can attain large sizes so as to cause facial disfigurement. Generally underlying radiological changes cannot be seen but in rare instances if the lesion grow larger size there can be mild erosion of bone seen.11
To find out the etiology of the lesion, two theories have been postulated.6
The first one states that the lesion initially arise as a pyogenic granuloma and in later stages gets calcified.
The second theory state that it originates from an inflammatory hyperplasia in the cells of the periodontal ligament;
This second theory is fairly more accepted, since POF occurs exclusively in the gingiva and in close proximity to the periodontal ligament. Furthermore, there has been evidence of calcified matrix-rich oxytalan fibers included in the POF which supports the periodontal origin of the lesion.4, 12
Chronic irritation of the periosteum and the periodontal ligament causes metaplasia of the connective tissue, which results in bone formation and dystrophic calcification.5 Frequent irritation during exfoliation of deciduous tooth and eruption of permanent tooth eruption may also results in an increased incidence of POF.8
Clinical manifestations of POF include a reddish, a well-circumcised gingival lesion. Older lesion appear smooth pink surface. Lesion generally not exceed 3 cm. Sometimes it is associated with pain, and With the large sized lesion, displacement of teeth and ulcerations can be present as well.13, 14 The growth probably begins as an ulcerated lesion; older ones are more likely to demonstrate healing of the ulcer and an intact surface. Red, ulcerated lesions often are mistaken for pyogenic granulomas; the pink, nonulcerated ones are clinically similar to irritation fibromas.
The basic microscopic pattern of the peripheral ossifying fibroma is one of a fibrous proliferation associated with the formation of a mineralized product. If the epithelium is ulcerated, then the surface is covered by a fibrinopurulent membrane with a subjacent zone of granulation tissue. The deeper fibroblastic component often is cellular, especially in areas of mineralization. In some cases, the fibroblastic proliferation and associated mineralization is only a small component of a larger mass that resembles a fibroma or pyogenic granuloma.
The mineralized component in the lesion is variable and may consist of bone, cementum-like material, or dystrophic calcifications or a combination of products is formed. The bone usually is woven and trabecular in type, although older lesions may demonstrate mature lamellar bone. Some times trabeculae of unmineralized osteoid are also seen. It is less obvious that ovoid droplets of basophilic cementum-like material are formed. Dystrophic calcifications are more common in early, ulcerated lesions; older, nonulcerated examples are more likely to demonstrate well formed bone or cementum. Multinucleated giant cells may be found in some cases in association with the mineralized product.15
The treatment of choice is a excision of a lesion with histopathologic examination. The mass of the lesion is excised deep to the periosteum which lowers the chances of recurrence. The adjucent teeth should be thoroughly scaled and root planing is also done to remove irritant factor. Sometimes periodontal esthetic surgery require in esthetic area.
Case Report
A 19-year-old female patient came to the department of periodontology with chief complain of swollen gum in lower right anterior jaw region since 4 months(Figure 1)
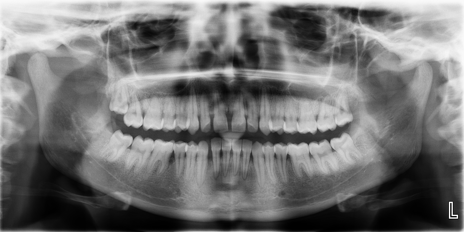
No deleterious hygiene habit found and oral hygiene status was poor. The lesion appeared sessile growth, pink in colour with smooth surface and 1cm × 1m in size at lower right canine and first premolar region. Radiograph of the lesion showed localised bone loss between 43 and 44 region (Figure 2)
After through scaling and root planing is completed, the excision of the lesion is planned. Pre operative 10% Povidone Iodine apllied to the skin around oral cavity for preventing contamination. 0.2% chlorhexidine gluconate mouth rinse was performed by a patient before the surgery to lessen the load of microbiota in oral cavity. Topical anesthetic with 15% lignocaine spray apllied at the injestion site. Anesthesia was performed by local infilteration with 2% lignocaine with 1:1,00,000 adrenaline. After proper anesthesia is achieved the excision of the lesion is performed and the lesion is immediately stored in 10% formaline and transfered for the histopathologic examination. Hemostasis at the site was achieved and the area was throughly evaluated for wheather the local irritant was present and the adjucet teeth were thoroughly scaled and root planing was performed. Surgical site was protected by coepak. Periodontal dressing was removed after 10 days(Figure 3).
Histopathologic examination with H&E stain revealed dense connective tissue stroma with plump proliferating fibroblasts and regularly arranged collagen fiber bundles. The stroma reveals presence of normal bony trabeculae lined with osteoblasts with osteocytes within. Also numerous well circumscribed cementum like materials was noted in form of ossicles dispersed in the stroma. Also numerous blood vessels with extravasated RBCs were noted. The overlying epithelium was hyperplastic with hyper parakeratinized stratified squamous epithelium(Figure 4).
These clinical, radiographic and histopathological findings are suggestive of peripheral ossifying fibroma.
Discussion
It has been suggested that the POF represents a separate clinical entity rather than a transitional form of pyogenic granuloma, PGCG, or irritation fibroma. Eversole and Rovin2 stated that as compared to pyogenic granuloma and peripheral giant cell granuloma with the similar sex and site predilection and clinical presentation, POFs having a varied histologic response to irritation. Kfir et al. reported that the size of the POF is usually smaller than 1.5 cm in diameter. Although a case of giant POF of 9 cm is reported in the literature.16 Gardner stated that POF cellular connective tissue is so characteristic that a histologic diagnosis can be made with confidence, regardless of the presence or absence of calcification.3 Buchner and Hansen hypothesized that early POF presents as ulcerated nodules with little calcification, allowing easy misdiagnosis as a pyogenic granuloma.17 The hormonal influence especially with estrogen and progesterone is associated with high prevalence in female patients, since the variation in their levels can be reflected in puberty and pregnancy, so that the POF prevalence during the second decade in female patent can be higher.18
Multicentric POF can also occur in oral and maxillofacial region and is observed in genetic associated conditions like:19
Conclusion
As there are so many gingival lesions with similar gingival presentation, Histopathological examination is necessary to confirm the diagnosis of Peripheral Ossifying Fibroma. Clinical presentation of this case in female patient in her 2nd decade of life, satisfy with the frequent appearance of the lesion. Radiograph shows superficial erosion of bone. But the histological section confirms the diagnosis of POF. POF resemblance PGCG, pyogenic granuloma, and irritation fibroma; hence, thorough knowledge of the difficult diagnosis and specific lesion is important to draw a conclusion.