Introduction
Oral submucous fibrosis is chronic disabling disease with obscure etiology that affects the complete oral cavity occasionally with the pharynx, and rarely involving the larynx. It is characterized by blanching and stiffness of the oral mucosa, which causes progressive limitation of mouth opening and intolerance to hot and spicy food.1 Its precancerous nature was described by Paymaster, who recorded that, in one third of patients with squamous cell carcinomas has a slow onset of growing. Murti et al.2 reported the malignant transformation of oral submucous fibrosis. The purpose of this report is to examine the experience and results obtained with the use of reconstruction of intraoral defects with PMF. The PMF was described in 1970 by Paul Tessier. It was first used for reconstruction of intraoral defects by Futrell in 1978.Reconstruction of small to medium oral soft-tissue defects with PMF is in use since last 30 years(Ariyan S 1997).3 It is mainly used in the reconstruction of soft tissue defect of parotid,buccal mucosa,ear,chin,lip& pharyngeal wall. It seems to be an excellent choice particularly in medically compromised patients not being eligible for free tissue transfer. After resection of carcinomas of head and neck require functional reconstruction either with the tounge flap, nasolabial or either from PMMC flap, latissimusdorsi flap, trapezius flap but these can be used at the selected areas and are bulky flaps. Platysmamyocutaneous flap was first used in 1887 by a surgeon of Austria Robert Gersuny to close the full thickness cheek defect since then it is in use in oral functional reconstruction after carcinoma or other dysplastic growth resection or in oral sumucous fibrosis patients (Cannon, et al., 1982).4 Since there is no definitive surgical treatment of SMF as every treatment modality has its own drawbacks ,PMF can be safely used in the reconstruction of excised fibrous bands in SMF patients. Its use in reconstruction was not so much advocated as its arterial and venous supply can be hampered during its dissection.5 PMF can either be superiorly based, posteriorly based or inferiorly based, mainly oral and facial defects are reconstructed with superiorly based flap.6 This flap has got robust blood supply from facial & submental arteries, apart from this from superior thyroid artery medially, occipital artery and posterior auricular artery laterally and transverse cervical vessels inferiorly. Submental artery is the main feeder vessel for superiorly based PMF. Main disadvantage is its inadequate venous drainage which is through anterior small communicating veins which drains in to superior thyroid vein, anterior jugular vein or facial vein.this is due to the venous drainage pattern which is vertical and superficial. 7 On the other hand posteriorly based flap has inadequate arterial supply which is through random pattern occipital artery while this is having adequate venous drainage through external jugular vein.This flap can be used in medically compromised patients where free tissue transfer can not be done.This flap is contraindicated in patients with prior neck incisions , previous radiotherapy, and prior exposure to neoadjuvant chemotherapy.8 This flap is having thin pliable tissue which can be rotated intraorally to reconstruct cheek defect along with skin .We think that platysmamyocutaneous flap is a better option that an extended nasolabial flap in terms of extraoral facial scar for the management of oral submucous fibrosis.
Here we present a study where 8 cases of platysma flap were done in the lesions where incisional biopsy was presented as oral submucous fibrosis with predictable outcome.In our study there were 8 patients in whom platysma flap was done, in two flaps there was venous congestion which was managed conservatively and all the flaps remained viable.
Materials and Methods
From the year 2017-2018,8 cases of SMF who underwent superiorly based platysmamyocutaneous flaps were undertaken in the department of oral & maxillofacial surgery, King George medical university, lucknow. Patients were in the age group of 40 – 50. Among them 7 were male patients and one female patient. All the 8 patients were having biopsy report of oralsubmucous fibrosis, in which after band resection PMF was done. Clinically the patients were in grade III and IV of oral submucous fibrosis with fibrous bands palpable over bilateral retromolar region extending though buccal mucosa up to commissure of mouth.
Surgical procedure
The neck of the patient is hyperextended, to begin with the procedure the fibrous band resected area in the oral cavity was measured so as to determine the length of skin paddle to be used. A maximum of 6*10 cm can be harvested(Figure 1).The elliptical incision is then given to harvest skin paddle lower in neck above the clavicle .It depends mainly on length of the flap to be harvested to reconstruct the area anterior or posterior in oral cavity. The superior margin of the incision is in the subdermal plane superior to the platysma muscle which was dissected while the inferior margin is deep to the platysma muscle(Figure 2). Dissection should be started 1 cm below the marked inferior margin of the skin paddle so as to save the perforators.
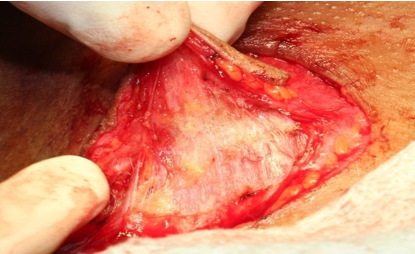
After dissection of the vessels which were present in the cervical facia with in or close to the platysma muscle, the flap is then developed in the subplatysmal plane including the investing layer of deep cervical fascia (Figure 3). Vertical incision is given in platysma muscle both anteriorly and posteriorly of the flap so as to have proper mobilization. Dissection was then carried up to 2cm below the lower border of the mandible so as to protect the facial vessels as they emerge from the submandibular gland.
Flap is then rotated so as to place over the defect with out stretching or compressing it. Wide tunnel intraorally is then created so as to place the skin paddle at the lesion resected area and suturing is done (Figure 4).
Care should be taken to protect the external jugular vein for proper drainage and protection of submental and facial arteries also and to protect the flap from excessive tension and kinking. The harvested platysma flap should be around 4 cm in width. Only from a single elliptical incision whole of the PMF was harvested through dissection upto the level 2 cm below the lower border of mandible, providing a uniqueness to the study with improved cosmetic result.
Results
The patient population was evaluated for immediate and delayed postoperative complications, with follow-up ranging from 6 months to one years. Out of 8 patients in whom the PMF was done, 2 patient had venous congestion of the flap which then resolved in 72 hours in one patient while 1 patient developed secondary epidermolysis of distal 1 cm of skin of flap which was managed by debridement and secondary healing. All flaps survived with no failure and all the patients had good cosmetic result intraorally with no donar side complications (Table 1).Nasogastric tube feeding was maintained during the firstweek after surgery.
Table 1
SMF patients who underwent superiorly based PMF
Discussion
Superiorly based PMF is used in this study to reconstruct the mucosal defect created after resection of the bands in case of oral submucous fibrosis. All the flaps remained vital during 6-12 months follow up. Though in 2 cases venous congestion was developed which resolved in 72 hours which must be due to development of other draining channels. In previous studies Conley et al,9 it is mostly used to reconstruct the mucosal or skin defect created by resection of the oral carcinomas which resulted in about 40% of the failures of the flap when reconstructed simultaneously, which was mainly due to ligation of facial artery and cauterization of submental arteries but in studies done by In contrast McGuirt et al.10 found that only 1 in 20 patients who had thefacial artery ligated had partial loss of the flap’s surface. In one study it was seen that there was no failure of flap even in the cases where in whom resection of the carcinoma was done with simultaneous placement of PMF, this was mainly due to retrograde supply due to anastomosis of distal submental branches to the facial or lingual arteries of the contralateral side. In one of our cases there was skin loss in distal part of the flap which must be either the perforating veins were violated during harvesting of flap or the perforating veins were not present in that part of the flap.
For taking superiorly based PMF in reconstruction of intraoral defects one should consider following points like preoperative radiotherapy which results in damage of microvascular supply of skin of neck, preoperative neoadjuvant chemotherapy and level 1 neck dissection itself because it leads to diatherming submental vessels which leads to compromised blood supply and inadequate drainage. These might be the reasons associated with previous studies in whom there was least success of PMF.
The success of PMF mainly depends on dissection in a proper plane, if flap is incorporating platsma muscle along with the investing layer of deep cervical fascia then there are least chances of violating arterial or venous supply. 11 During turning of the flap to its required position care should be taken not to put excessive pressure on the arteries or veins which might result in inadequate perfusion and venous congestion.
Various other surgical modalities for management of SMF patients carries with them some or other drawbacks like resection of the fibrous bands and recommending physiotherapy to the patients allowing for secondary epithelialization often results in rebound fibrosis.Palatal island flap recommended by Andrade has difficult reach and for it second molar is to be extracted.
Toungue flap most often results in dehiscence because of tongue movement and there is often risk of aspiration. Split thickness skin graft most commonly results in contracture development.
Buccal fat pad has its own disadvantages because anterior defects i.e in region of canine can not be reconstructed because of difficulty of reach which further results in fibrosis. Extended nasolabial flap results in ugly scar over face so canot be used in young patients.
In comparision to all these flaps if dissection of PMF is done in proper plane and if the arterial and venous supply is not violated there are least chances for the failure of the flap. One thing should be kept in mind that in patients in whom there is thin platysma muscle PMF should not be undertaken as the blood supply of PMF is more faciocutaneous as compared to musculocutaneous. Besides this cosmetic results are good as there is no extraoral scar and the donar site scar is always behind the collar.