Introduction
When looking into odontogenic cysts (OCs), dentigerous cyst (DC) is the epitome of developmental OCs. By definition, “DC is an odontogenic cyst that is attached to the cervical region of an unerupted tooth and envelops the crown” according to the WHO 2017 classification of Head and Neck Tumors.1 DC is the most frequently occurring developmental OC and is second to a radicular cyst (RC) in incidence when considering all the OCs combined. DCs comprise approximately one-fourth of all the cysts of the jaws. The cyst tends to occur in younger individuals with a peak of occurrence in second to fourth decade of life.2 There is a slight male predilection and a marked propensity to occur in the mandibular posterior region.
The most pathognomonic feature of DC is associated with an impacted tooth and the cystic wall being attached to the cementoenamel junction of its crown.3 A thin lining of odontogenic epithelium lines the luminal surface of the cystic cavity into which the tooth projects. It has been reported that DC forms in about 1.44 out of every 100 unerupted teeth.4 In about 5-6% of these cases, the cyst may also be associated with a supernumerary tooth rather than that of a normal series.5
The exact pathogenesis of DC is yet uncertain but it is widely believed that the cyst arises due to an accumulation of fluid between the reduced enamel epithelium of the dental follicle and the crown of the unerupted tooth.6 Therefore, the cyst is also called as ‘follicular cyst’, and an unerupted tooth is a sine qua non for its formation.
Herein, we report a case of DC occurring in an 11-year-old male along with is surgical management.
Case Report
An 11-year-old male complained of pain in the right mandibular posterior region since three months. The pain was dull and had a spontaneous onset. It was initially of mild intensity but gradually progressed over time to become severe. The pain got aggravated by chewing food and sleeping, while it was relieved by taking analgesics. The patient’s medical history was unremarkable and there was no episode of previous physical trauma. A history of pulpectomy followed by stainless steel crown coverage was elicited with deciduous maxillary left and mandibular right second molars.
A diffuse swelling approximately of size 3 x 3.5 cm was noted involving the right lower third of the face (Figure 1 A). The swelling extended from the right corner of the mouth up to 1 cm anterior to the right tragus. Intraorally, a diffuse expansion of the buccal cortical plate in the region of the deciduous mandibular right second molar; while the tooth exhibited grade III mobility. A prior history of endodontic treatment with stainless steel crown coverage two years ago was elicited with respect to the same tooth. The crown of the permanent mandibular right first molar was grossly destructed due to caries and there was an overgrowth of the surrounding soft tissues into the tooth on its lingual aspect (Figure 1 B).
Figure 1
A)Extraoral swelling involving the right lower third of the face; B) Grossly carious permanent mandibular right first molar

Figure 2
Orthopantomogram showing a well-defined unilocular radiolucency surrounding the neck of the crown of the unerupted mandibular right second premolar
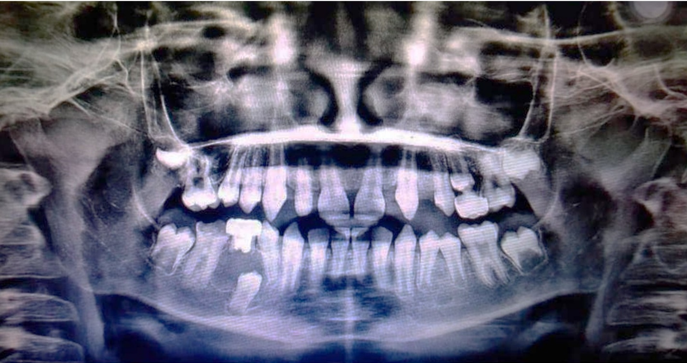
Figure 3
A) Extracted mandibular right permanent first molar and deciduous second molar; B) Enucleated lesion in toto
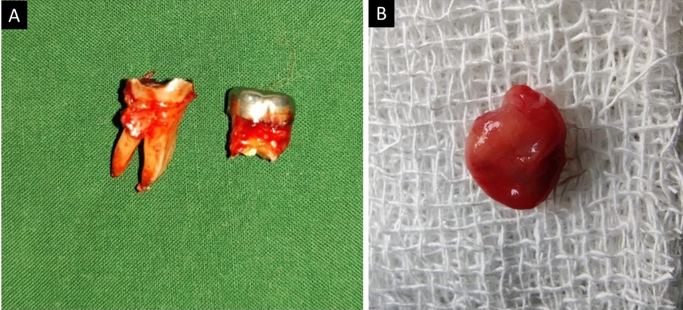
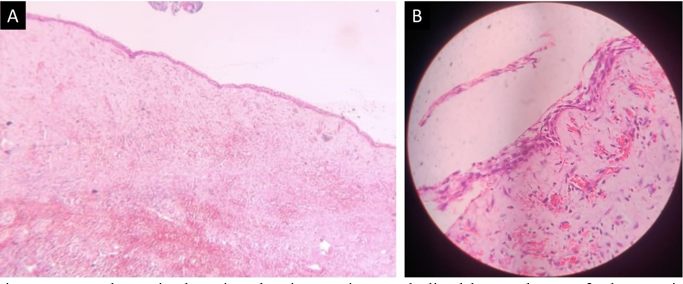
Figure 4
H and E-stained section showing cystic capsule lined by 2-4 layers of odontogenic epithelium in A) Original magnification x40, and B) Original magnification x400.
Orthopantomogram (OPG) revealed a well-defined unilocular radiolucency surrounding the neck of the crown of the unerupted mandibular right second premolar with diffuse and thin corticated borders (Figure 2). Severe caries affected the enamel, dentin, and pulp of the permanent mandibular right first molar. Resorption of more than two-thirds of the root of the deciduous mandibular right second molar was also noted. The mandibular right first premolar exhibited distal tipping owing to the pressure from the lesion distal to its root position.
The working diagnosis was considered to be ‘dentigerous cyst’; while the differential diagnosis included RC, odontogenic keratocyst (OKC), unicystic ameloblastoma (UAM), adenomatoid odontogenic tumor (AOT), and calcifying epithelial odontogenic tumor (CEOT). The involved molars were extracted and the lesion was enucleated in toto.
Histopathology revealed a cystic lumen lined by 2-6 layers of hyperchromatic odontogenic epithelium (Figure 3). The epithelium-connective tissue interface was flat. The cystic capsule comprised loose bundles of collagen fibers interspersed with plump to spindle-shaped fibroblasts. The capsule was devoid of any inflammatory infiltrate but showed some extravasated erythrocytes.
In line with the clinical presentation, radiographic features, and histopathological picture, a final diagnosis of DC was imparted for the case.
Discussion
Given the gross carious involvement and prior history of endodontic treatment in the lesional area, an inflammatory OC such as RC was included in the differential diagnosis of the present case. Even so, RCs seldom occur associated with primary teeth in younger patients.7 Additionally, the position of the lesion did not seem to lie periapical and its association with an impacted second premolar was more suggestive of DC.
Although the association of a radiolucency surrounding an impacted tooth is a characteristic of DC, it is not pathognomonic for the entity. The clinicians must be cautioned against directly diagnosing such cases as a DC as other odontogenic lesions such as AOT, CEOT, and UAM have been reported to occur in association with the crown of an impacted tooth in a significant percentage of cases.1, 3, 8 Furthermore, since the OPG provides only a two-dimensional view, the possibility that the lesion exists lateral to the tooth and is superimposed on its crown in the radiograph cannot be overlooked. In such scenarios, OKC, UAM, or CEOT could also be a possible diagnosis. One-third of CEOTs have been described to be associated with an impacted tooth and appear completely radiolucent rather than having the characteristic ‘snow driven’ appearance.3, 8 Biopsy must be considered mandatory to resolve the differentials before imparting a final diagnosis.
The impacted tooth is usually the mandibular third molar in about 75% of cases of DC.1, 9 Less frequently other teeth may be involved including maxillary canine, maxillary third molar, and mandibular second premolar, in the descending order of frequency. This order of frequency also corresponds to the frequency of impaction of the respective teeth. The hydrostatic pressure that develops within the lumen of a DC owing to the accumulation of fluid over time, has some pressure-related effects on the surrounding bone and the adjacent teeth.6 Therefore, DCs tend to be expansile and cause root resorption of the adjacent teeth; more so than other developmental OCs such as OKC.10 Herein, whether the mobility noted with respect to the deciduous second molar above the lesion could be fully attributed to the resorption caused by the cyst is questionable. It could also possibly be physiologic mobility given the age of the patient and no effect on the roots of any other adjacent tooth.
Considering the pathogenesis rationally, DCs cannot recur following their removal since the mechanism of fluid accumulation gets disrupted.1, 2, 3, 4, 5, 6 Therefore, simple surgical enucleation is considered to be adequate for the treatment of DCs. In the present case, there was adequate healing and no evidence of disease after six months of follow-up. Gauging from the position assumed by the premolar, eruption in a normal manner could be expected in future.
Conclusion
Although common and easy to diagnose, one must proceed with caution while diagnosing a DC as the clinical and radiographic features overlap significantly with other odontogenic cysts and tumors. Timely intervention can enable the associated teeth to erupt normally, thereby eliminating the need for additional rehabilitation for the patients. This ultimately improves the patient’s quality of life, given their young age in most cases.
