Introduction
Tooth displacement can happen when the direction and intensity of the force is sufficient to tear the periodontal ligament and fracture the dentoalveolar bone with or without tooth-root fracture. Based on the intensity of force, it may result in other possibilities like subluxation or avulsion. Generally this results in non vitality of the tooth. The management to preserve the tooth depends on its magnitude and extent of the injury. This article is about a case report presented to us with displaced central incisor into the frontal sinus due to RTA. We also discuss about the mechanism of tooth displacement, extent of injury to the neighbouring structures, its associated complications and its management.
Case History
A 45 year old male reported to our emergency room with history of RTA. His level of consciousness evaluated through Glasgow Coma Scale (GCS) being 12/15. He presented with generalized edema on his mid face with missing two upper central incisors and one lateral incisor. He also suffered soft tissue tear involving the nasal region and lower lip. Hemostasis was achieved primarily by suturing the soft tissue injuries. He also presented with CSF rhinorrhea with halo sign positive.1
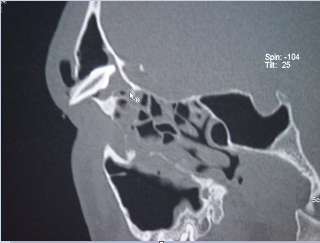
The patient was stabilized. Computer tomography (CT) brain and CT facial bones were taken which revealed dentoalveolar fracture of maxilla, avulsion of right central and lateral incisors and displacement of left central incisor into the frontal sinus [Figure 1]. The tooth displacement also caused soft tissue tear of the nasal floor puncturing the nasal septum and fracturing the outer table of the frontal sinus. The injury extends to the cribriform plate of ethmoid bone resulting in CSF rhinorrhea.
The patient was managed with triple antibiotic protocol (IV. Ceftriaxone and Sulbactam, IV. Amikacin and IV. Metronidazole 12th hourly) as a prophylactic measure for meningitis,2 intravenous (IV) manitol and epsolin, as he was in a irritable state due to Traumatic Brain Injury (TBI). The CSF rhinorrhea subsided after 48 hours.
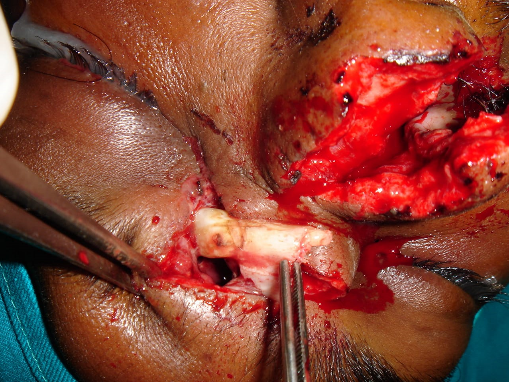
The patient was taken up for surgery after 48 hours. Through the existing laceration on his fronto-nasal region the displaced central incisor was identified and removed [Figure 2]. Thorough wound debridement was carried out. The obliterated frontal sinus was debrided and packed with gelfoam. Titanium mesh was placed to mask the defect over the frontal sinus. The nasal septum and lateral nasal cartilage was sutured with 4-0 prolene followed by soft tissue closure with 3-0 ethilon. To maintain the patency of the nostrils, nasopharyngeal airway tubes were placed in either of the nostrils for a week. The length of the nasopharyngeal airway was shortened to minimize the discomfort for the patient. The patient recovered well. Patient did suffer from partial anosmia. His ocular movements were normal. No paresthesia on the facial region.
Discussion
The cranium facial complex in relation to the extra oral tooth displacement in maxilla is surrounded superior-medial by the nasal cavity, superior-lateral by the maxillary sinus cavities. Superior to that he presence of orbital cavity on both sides along with the cranial cavity.3 Based on the tooth displacement which can cause injury to the neighbouring structures resulting in loss of function like disturbance in ocular functions and anosmia,4 infections to the dangerous area of the mid face leading to cavernous sinus thrombosis,5 further spread leading to meningitis. Other signs can include CSF rhinorrhea and sinusitis.6
Principle of mechanism of the injury
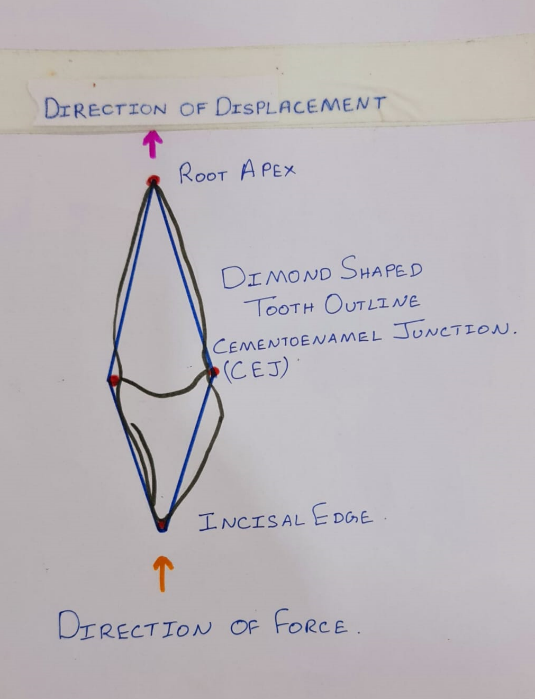
The outline of displaced central incisor can be compared to a diamond shape with the root apex long and pointed at one end and the incisal edge of the crown flat at the other with widest part at the middle being the cementoenamel junction (CEJ). [Figure 3] With sufficient force parallel to the angulation of the tooth which makes it a perfect projectile to get displaced into the neighbouring anatomical structures of the face. In our case the central incisor managed to pass through the alveolar bone, nasal cavity, puncture the nasal septum, fracture the fronto-nasal junction, fracture the outer table of frontal sinus and damage the cribriform plate of ethmoid bone leading to CSF rhinorrhea.
With proper assessment and radiographic evaluation we can diagnose the presence of displaced tooth or foreign body into the neighbouring facial structures. In such scenario involving the fronto-nasal region careful assessment of intra cranial region through CT brain to rule out extra dural hemorrhage or sub dural hemorrhage, CSF leak, patient level of consciousness by GCS, pupillary reflex is important. Prophylactic intravenous antibiotics should be started well before the surgery. Neuro physician / neurosurgeon opinion must be taken to assess the patient to decide when to be taken up for surgery. In our case we delayed the surgery by 48hrs as the patient was irritable due to edema of the brain as a result of TBI. He didn’t suffer any intra cranial bleed which required immediate intracranial decompression procedures. In cases where intra cranial procedures are required joined team approach between neurosurgeon and maxillofacial surgeon may be required.