Introduction
Patients’ increasing demand for aesthetic restorations have led to a rapid development in the field of resin-based composite materials.1 The final aesthetic appearance for any composite restoration depends on the artistic ability of the clinician, the contouring shaping of the restoration and the finishing and polishing of the restoration. Effective finishing and polishing of composite restorations provide optimal aesthetics, acceptable oral health of soft tissues and marginal integrity of the restorative periodontal interface.2 The bacteria, especially Streptococcus mutans (S. mutans), play an important role in the initiation pathogenesis of secondary caries since these are the pioneer colonizers in the biofilm. They have high affinity for adhesion, responsible for surface damage and biodegradation of resin restorations. It is well established that material surface roughness is a key factor that makes composites vulnerable to bacterial adhesion and biofilm development. A rough, unfinished, and poorly polished composite surface is more likely to accumulate plaque. Different polishing kits are commercially available like carbide and diamond burs, abrasive discs, abrasive strips, abrasive-impregnated rubber cubs and points & finishing and polishing pastes. Chairside polishing of the composite restoration is important for an aesthetic appearance as well as a smooth polished surface with less biofilm formation. If finishing and polishing procedures are done before the adequate time required for achievement of complete polymerization, physical properties of composite are affected and might increase the possibility of early failure of restoration.3 The hardness of the composite materials depends on the amount of filler, composition, resin type, the depth and time required for complete polymerization.
Hence, this study aimed to assess the Streptococcus mutans adhesion and microhardness of composite after polishing them with two different polishing systems immediately and after 24 hours of curing. The null hypothesis was that there will be no difference in bacterial adhesion and microhardness of composite after polishing with two different polishing systems immediately and after 24 hours of curing.
Materials and Methods
The present study was carried out using nanocomposite Filtek Z350XT (3M ESPE, St. Paul,MN, USA) blocks that were subjected to finishing and polishing. Polishing treatment (three levels: control, polishing performed immediately and delayed after 24 hours of storage) were performed by two polishing systems Sof-Lex (3M ESPE) and Super- Snap (Shofu Inc., Kyoto, Japan).
Table 0
The experimental units were then divided to check for two parameters. One was subjected for incubation to check for bacterial biofilm adhesion and the other for microhardness testing.
Sample preparation
A cylindrical shaped Teflon mold of dimensions 6mm×4mm was custom made for preparing the composite blocks. The mold was filled in with a single increment of the nanofilled composites Filtek Z350XT (3M ESPE, St. Paul,MN, USA) cured by placing over a Mylar strip for 40 seconds in a curing unit device EliparTM DeepCure-S LED curing light (3M ESPE, St. Paul, MN, USA) with a light intensity of 1470 mW/cm2 for 40 s, according to the recommendations of the manufacturers. Composite resin blocks (n=60) were then randomly divided into 3 groups according to the polishing system used.
Polishing treatment and time
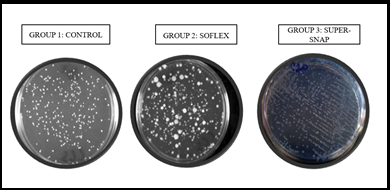
GROUP 1(n=20)- CONTROL (the Mylar strip, and no finishing or polishing procedures were performed).
Subgroup 1a (n = 10)- without salivary incubation.
Subgroup 1b (n = 10)- incubation for 24 hours in artificial saliva.
GROUP 2 (n=20)- SOF-LEX (3M ESPE Dental Products St. Paul, MN, USA.)
Subgroup 2a (n = 10)- polishing immediately
Subgroup 2b (n = 10)- polishing after 24 hours of storage in artificial saliva at 37℃
A sequence of four sandpaper discs (Sof-Lex coarse: 100 µm; medium: 29 µm; fine: 14 µm; and superfine: 5 µm)
GROUP 3 (n = 20)- SUPER- SNAP (Shofu Inc., Kyoto, Japan)
Subgroup 3a (n = 10)- polishing immediately
Subgroup 3b (n = 10)- polishing after 24 hours of storage in artificial saliva at 37℃.
A sequence of four sandpaper discs (Super-Snap coarse: 80 µm; medium: 29 µm; fine: 14 µm; and superfine: 5 µm).
For groups B and C, polishing was done for 30 seconds/disc in a single direction under constant cooling with a water jet. At each disc exchange, the composite surface was washed and air dried for 5 seconds. A new polishing disc was used after every fifth sample.
Adherence testing was done under strict aseptic conditions.
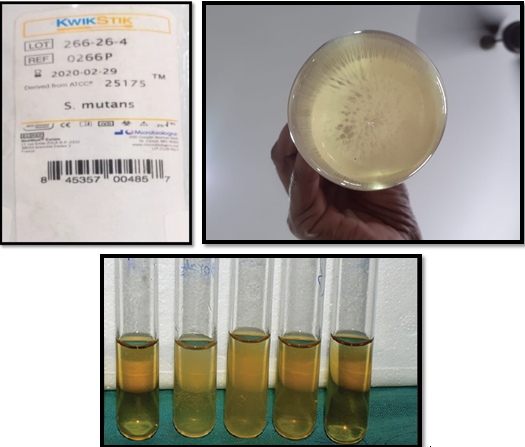
Inoculation of streptococcus mutans
Freeze dried Streptococcus mutans (ATCC 25175) obtained from ATCC 25175, HiMedia, Lot No. 266-26-4 was regenerated by dissolving in 10 ml of Brain Heart Infusion Broth (B.H.I) in conical flask, vortexed and incubated in Candle jar, in an incubator for 48 hrs. A standard suspension of Streptococcus mutants was prepared and was used as inoculums. Turbidity of standard suspension adjusted to Mc Farland 0.5 turbidity standard (5x108cells/ml).
Bacterial adhesion assay- (half of the samples of each sub-group n= 5)
Each composite block before incubation were decontaminated by soaking in 70% alcohol for 5 minutes. 1.5 ml of B.H.I. broth and 0.1 ml of standardized S. mutans suspension was added to polystyrene tissue culture plate. The plates were sealed and incubated at 37°C for 24 h in a CO2 jar. Samples were then removed and washed thrice with a sterile PBS (Phosphate Buffer Solution) to dislodge loosely bound material. Following this, samples were placed in tubes with 3 ml of sterile physiological saline (0.9%) and sonicated (Sonoplus HD 2200, 50 W, Bandelin Electronic, Berlin, Germany) for 30s to disperse the biofilms. The suspension obtained was diluted at 100 times and aliquots were made and 0.1 ml from each aliquot was then seeded on BHI agar to see the number of colonies after 24 h incubation at 37°C. Mean values of colony forming units (CFU) were noted by colony counter (Phoenix CP-600, Sa˜o Paulo, Brazil). The dilution of S. mutans was done to avoid the false results of biofilm adherence, as the organism has a property of formation of biofilm due to coaggregation.
Micro Hardness Testing(other half of the samples n=5)
Micro hardness of every specimen was determined using a micro-hardness tester (Micro-vickers hardness tester,Wolpert group, China) equipped with a diamond Vickers indenter. The indentation load was 0.1 N and the dwell time was 10s. Three indentations spaced equally over circle were made on the surface of each specimen.
Statistical analysis
For bacterial adhesion, mean values of CFU/mL were converted into logarithmic (log10) values and analyzed by a three-way of variance ANOVA. A p value <0.01 was considered to indicate a statistically significant difference.
For microhardness of composite, effect of the immediate and delayed finishing/polishing analysed by two-way ANOVA showed a statistically significant value (p < 0.01).
Results
Mean and standard deviation values of the CFU/ml (log10) of S mutans within the biofilms formed and microhardness values displayed in Table 2, Table 3.
After 24 hours of salivary incubation increased bacterial adhesion on composite (Filtek Z350XT) regardless of polishing treatment performed (p<0.01).
The Control group (Mylar Strip) presented the lowest bacterial adhesion (p< 0.01).
For delayed polishing (after 24 hours) Super-Snap (sub group 3b) showed highest bacterial adhesion than Sof-Lex (sub group 2b).
Table 1
Data displaying mean and SD (Standard Deviation) values of the CFU/ml (log10) of Streptococcus mutans within the biofilms on composite after polishing them immediately and delayed (after 24 hours) with different systems
Discussion
Proper finishing and polishing of composite restoration have been related to less plaque retention, subsequently decreasing the rate of secondary caries and marginal discoloration, thus enhancing the aesthetics and longevity of the restoration. Surface roughness is one element that makes resin based composite materials susceptible to bacterial attachment and biofilm formation.4 Previous studies have proposed that a surface roughness value of 200 nm is the upper limit for bacterial retention.5 Thus, considering that microorganisms have a higher affinity for resin composites in comparison to the enamel and other restorative materials,6 studies involving microorganisms’ attachment to resins surfaces are relevant. Surface roughness can be expressed as a function of the microrelief of the surface created during the finishing and polishing procedure.7 Immediate polishing leads to abrasion of softer resin matrix leaving the harder filler particles due to incomplete polymerisation, production of high localized heat8 and scratch lines left by abrasives of greater size.9 The microrelief of the surface especially voids, cracks and pits are of critical clinical relevance as it has been reported to create protected sites for bacteria.10 Finishing and polishing composite can minimize plaque accumulation, subsequent marginal tissue inflammation, and recurrence of caries while improving wear behavior and the marginal integrity of restoration.11
Due to heterogeneous nature of dental composite, for effective polishing an abrasive should remove the softer resin matrix as well as cut the relatively harder filler particles. Sen et al. stated, the polishing of methacrylate resin matrix produced the smoothest surface than the bisacryl resin matrix due to the presence of a homogenous composition. 12 Nanocomposites like Filtek Z350XT composed of nonagglomerated 20-nm nanosilica filler and loosely bound agglomerated zirconia/silica nanoclusters, which consists of agglomerates of primary zirconia/ silica particles with a filler size of 5-20 nm, have better handling properties and used clinically as a universal restorative material for both anterior and posterior surfaces. In this study lower streptococcus mutans biofilm adhesion was observed on Filtek Z350XT after finishing and polishing, which is due to the reduced roughening owing to smaller size and the wide distribution of the fillers. 13, 14
Studies stated that curing composites against a Mylar polyester strip (Du Pont Co., Wilmington, Del.) produced the smoothest surface and the surface had a high glossy finish. 15, 16 This surface is rich in unpolymerized resin matrix alone and when exposed to oral environment may undergo degradation exposing the filler particles. This increases the rate of plaque accumulation and degradation of the restoration. Therefore, finishing and polishing of the surface of a resin composite restoration is critical in the clinical success. In many studies, a resin composite, polymerized against a Mylar strip, was used as a control. 17 Although Mylar strip provides the smoothest surface, in clinical settings, restorations routinely require final treatment for contouring, occlusal adjustment, and the removal of excess material. Due to its high resin content, the layer cured in contact with the strip is more susceptible to wear, and should be removed. 18 Stoddard and Johnson suggested that the material itself, filler size, content, type of abrasive used, number of strokes, amount of pressure applied, time spent on each abrasion, direction of the abrading surfaces, and geometry of the abrasive instruments impact the effectiveness of finishing and polishing systems. 19
Extrinsic factors like flexibility of the material in which the abrasives are incorporated, the hardness of the abrasives, the geometry of the instruments, and the way they are used are associated with the type of polishing system used. 20, 21, 22 Many studies reported that aluminium oxide discs gave smoother finish than diamond and silicon carbide polishing systems. 7, 23, 24 Moreover, delayed polishing showed lower surface roughness values because immediate polishing leads to removal of excess softer organic matrix leaving the harder filler particles on the surface before complete polymerisation could take place. Sof-Lex and Super Snap polishing systems are composed of aluminium oxide particles, which abrade the resin matrix and filler particles simultaneously during polishing. If finishing and polishing procedures are done before the adequate time required for achievement of complete polymerization, physical properties of composite are affected and might increase the possibility of early failure of restoration. 25 Bacterial adhesion is not only influenced by the physical and chemical composition of composites, but also by the material type, polishing medium, finishing and polishing time, technique performed, and the presence of saliva pellicle.
Hence in the present study, Streptococcal mutans adhesion on the composite blocks after immediate and delayed polishing was assessed.
In the study, delayed polishing showed lower bacterial adhesion because immediate polishing leads a more roughened surface due to removal of excess softer organic matrix leaving the harder filler particles on the surface before complete polymerisation could take place. Sof-lex showed less bacterial adhesion than Super-Snap with statistical significance (p <0.01). This may be due to the fact that the abrasive particle size in Super-Snap (ultrafine disc has particle size of 8μm) is larger than that of Sof-Lex (ultrafine is 7μm) and inability of Sof-Lex to displace filler particles in composite, thereby providing a homogenous abrasion of the fillers and resin matrix which promotes less bacterial adhesion. 26
The hardness of the composite materials depends on the amount of filler, composition, resin type, and the depth of polymerization. The overall hardness of the material is influenced by the monomers that do not participate in the curing process, which lower the hardness. The increased amount of inorganic filler also contributes to the hardness of the composite. 27, 28
In the present study, the control group (Mylar strip) showed lower microhardness values due the presence of excess organic matrix on the surface than those of properly polished surfaces. 29, 30 Delayed finishing/polishing significantly increased the hardness of the composite irrespective of the polishing system used. Moreover, in the present study, delayed polishing of the composite both Sof-Lex and Super-Snap had shown greater micro hardness values than immediate polishing. The results are in accordance with Yap et.al study where they concluded that polishing can give a more permanent deformation resistant surface but if polishing is performed without any delay after polymerization, due to partial maturation, composites are more prone to the effects of heat generation, in that way reducing their micro hardness.31 Delayed polishing is also supported by Lopes et al. where they suggested that a delay of 24 hours after polymerization for the initiation of polishing of composite resulted in a surface of similar or even harder than that obtained with immediate finishing/polishing. 32 Venturini et al. reported that immediate polishing did not produce a negative influence on the surface roughness, hardness and microleakage of a microfilled (Filtek A110) and a hybrid (Filtek Z250XT) resin composite compared to delayed polishing. 33
Conclusion
The reproduction of all in vivo conditions of the oral cavity for the analysis of biofilm formation is a very challenging process. So, within the limitations of this in-vitro study
Bacterial adhesion was least for control group-Mylar strip
Delayed polishing procedures for both polishing systems had significant difference on Streptococcal mutans adhesion than immediate polishing.
Micro hardness of composite was lowest in Mylar matrix group. Immediate polishing procedure showed lower microhardness values as compared to polishing that was delayed for 24hours for both polishing groups.
Therefore delayed polishing influences higher superficial hardness values of the nano-composite.