- Visibility 50 Views
- Downloads 13 Downloads
- DOI 10.18231/j.idjsr.2021.037
-
CrossMark
- Citation
Traumatic gingival fibroma of anterior maxilla: A case report
- Author Details:
-
Revati Niteen Deshpande *
-
Harshad Bhagwat
-
Ashvini Vadane
Introduction
Oral mucosa is constantly subjected to internal and external stimuli which may lead to localized inflammatory hyperplasia. Deley et al in 1990 gave the term Fibro epithelial hyperplasia. [1] The benign tumors of the fibrous connective tissue are called fibromas. [2] They were first reported in 1846. [3] A review of benign oral soft tissue tumors and bony prominences in white Americans older than 35 years old identified irritation fibromas as the 2nd most common benign oral lesion (12.0/1000). [4] They are usually small in size measuring approximately 1.5 cms or rarely more than that . Fibromas are generally slow growing, painless, solitary, sessile or pedunculated growths. They occur at any age but usually seen affecting patients in 3rd-6th decade. They are noted in 1.2% adults with 66% of female predominance. Causative factors are mostly thought to be trauma or irritation. There is reactive hyperplasia in response to trauma or local irritation which increases the size of an organ /tissue is responsible for most of the fibromas of the oral cavity. [5] Most of these lesions are reactive having varied appearance, but other developmental defects and neoplastic conditions are also noted in the gingiva, which gave rise to areas of clinical and also histological uncertainty in the diagnosis. [6] Traumatic irritants include restorations, calculi, foreign bodies, margins of caries, overhanging margins, chronic biting, sharp spicules of bones etc. [5] They commonly involve on buccal mucosa, tongue and gingiva. Palate is rarely seen to be involved because of less chances of trauma/ irritation. [2] This lesion does not have a risk for malignancy. [7]
Case Report
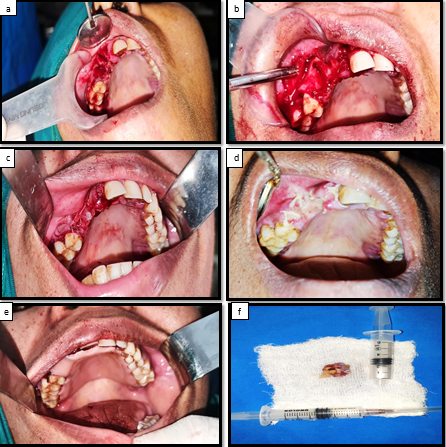
A female patient reported to the department of oral and maxillofacial surgery, aged 33 years with a chief complaint of slight pain and swelling in the right upper front tooth region. It was present since 15 days. Patient history revealed toothbrush trauma and the she noticed teeth mobility. On intraoral examination there was single, well circumscribed, firm, reddish pink swelling which was tender on palpation and located involving 13,14 buccally and 12,13,14 palatally and size was about 2.0 X 3.0 cm with pedunculated base.[[Figure 1]a,b,c]
Differential diagnosis
Periodontal abcess, Angiofibroma ,Keloids, Pyogenic Granuloma, Epulis Fissuratum, Neurofibroma, Gorlin Goltz Syndrome (Nevoid Basal Cell Carcinoma Syndrome, Verrucous Carcinoma Or Squamous Cell Carcinoma.
Investigations
OPG
Routine hematological investigations.
Excisional biopsy postoperatively gave a final diagnosis of gingival fibroma.

Treatment
The procedure was carried out under local anaesthesia. All aseptic precautions were taken. Local infiltration with 2% lignocaine with 1:2,00,000 adrenaline done around the lesion buccally and palatally. The lesion was completely excised using scalpel blade no.15 and electrocautery. 12,13,14 were extracted. Alveoloplasty was performed. Bony margins were smoothened using round bur. Hemostasis was achieved. Closure was done using 3-0 vicryl sutures and splint was placed. Patient was followed up at regular intervals. After 1 month the healing was satisfactory and there was no recurrence. [ [Figure 2] a,b,c,d,e,f]
Discussion
Fibromas are slow growing lesions and the growth is generally limited.[3] The growth potential does not exceed 10-20 mm and rarely exceeds 1.5 cm in size. [8] Trauma or irritation are found to be the causative factors. [3] Constant irritation from minor trauma ,masticatory forces, plaque, calculus, trapped food and debris, and iatrogenic factors, cause the gingival tissues react, leading to growth formation ,which was called by the Greek term epulis. [9] Barker and Lucas studied the pattern of collagen arrangement and depending on the site of the lesion and the amount of irritation, there are two types of patterns: (1) radiating (2) circular. They hypothesized that greater degree of trauma produces the radiating pattern which appears in sites which are immobile (e.g., palate), and lesser trauma produces the circular pattern and it occurs in sites which are flexible (e.g., cheeks). These lesions are usually asymptomatic. Such lesions, may also arise due to irritation by plaque microorganisms and local irritants and are clinically similar to peripheral ossifying fibroma, pyogenic granuloma and peripheral giant cell granuloma.[5] Each such condition must be subjected to biopsy for confirming the diagnosis as histopathological evaluation is the single most criterions for distinguishing them from each other. [10] Zhang et al found that carcinoma was included in the differential diagnosis in 2% of cases. Treatment consists of complete surgical excision and scaling of the remaining teeth. The patient must be followed up for a longer period of time because of the growth potential of incompletely removed lesions which was found to be 8%–20% and rarely recurrence is reported. [3]
Conclusion
Case report described here showed that treatment with scalpel blade and electrocautery was simple, safe and highly effective. No recurrence was noted after 1 month but a long term follow up is required and removal of trauma source or irritation is important to prevent the recurrence of the lesions.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- R M Sanadi, N Puppalwar, N Gurav, P Jain, P Khandekar. Fibroepithelial hyperplasia of Gingiva: A report of two cases. Med Res Chronicles . [Google Scholar]
- A Tsikopoulos. Large irritation fibroma of hard palate: a case report of a rare clinical entity. Pan Afr Med J 2021. [Google Scholar] [Crossref]
- N A Mohammed, S Chandrasekaran, M Valiathan. Fibroma of the Gingiva: A Case Report of a 20 Year old Lesion. IJCD 2010. [Google Scholar]
- T Esmeili. Common benign oral soft tissue masses. Dent Clin N Am 2005. [Google Scholar] [Crossref]
- G Jain, R Arora, A Sharma, R Singh, M Agarwal. Irritation fibroma: Report of a case. J Curr Res Sci Med 2017. [Google Scholar]
- D J Brierley, H Crane, D H Keith. Lumps and Bumps of the Gingiva: A Pathological Miscellan. Head and Neck Pathol 2019. [Google Scholar] [Crossref]
- J B Pai, R Padma, Divya, S Malagi, V Kamath, A Shridhar. Excision of fibroma with diode laser: A case series. J Dent Lasers 2014. [Google Scholar] [Crossref]
- J Desai, K Dave, G Bakutra, D Vasavada. Traumatic fibroma –A review and report of two cases. Int J Curr Res 2017. [Google Scholar]
- Y Kfir, A F Buchner, L S Hansen. Reactive Lesions of the Gingiva A Clinicopathological Study of 741 Cases. J Periodontol 1980. [Google Scholar] [Crossref]
- S Banerjee, T K Pal. Localized gingival overgrowths: A report of six cases. Contemp Clin Dent 2017. [Google Scholar]
