Introduction
Central giant cell granuloma (CGCG) is a benign, aggressive, destructive osteolytic lesion of osteoclastic origin.1 It was first described by Jaffe in 1953 and accounts for approximately 7% of all benign tumours of the jaws.2 Jaffe considered this tumour as a locally reparative reaction of the bone due to inflammation, local trauma or haemorrhage.3 The true nature of this lesion is controversial and remains unknown. The three competing theories are that it could be a reactive lesion, a developmental anomaly or a benign neoplasm. It usually appears as a solitary, multilocular, radiolucency, both in the mandible (mostly seen anterior to the first molars) and in the maxilla. It occurs at least twice as often in the mandible than in the maxilla, especially in females under 30 years of age. There are several reports of this lesion in other bones such as the sphenoid and temporal bones.4
CGCGs are classified into aggressive and nonaggressive lesions based on their biological behaviour, assessed by the presence of pain, rapid growth, perforation of the cortex, and a tendency to recurrence.5 Non aggressive lesions ranges from a slow growing asymptomatic swelling usually discovered on a routine radiographs.5 They are usually requires conservative surgical procedures.2 Aggressive lesions are characterized by one or more of the following features: pain, paraesthesia, root resorption, rapid growth, cortical perforation and a high recurrence rate after surgical curettage- between 37.5% and 70%.6, 7 These lesions that are mostly found in younger patients tend to be larger (over 5 cm) and require wide en-bloc resection that leads to major defects in the jaws that can alter the facial contours and necessitate major reconstruction. Some surgeons use autogenous bone grafts or vascularized fibula free flap for reconstruction of extensive CGCG. Non-aggressive lesions are In the literature, recurrence rates vary between 11% and 35% (72% of recurrence in the aggressive forms, 3% of recurrence in the non-aggressive forms).3, 8
Histologically CGCG appears as an intraosseous lesion consisting of fibro-cellular tissue, containing multiple foci of haemorrhage, aggregations of multinucleated giant cells, and occasional trabeculae of woven bone. 9
Differential Diagnosis that may be considered in such cases are Ameloblastoma, Schwannoma, Odontogenic cysts, Aneurysmal bone cyst, Chondroblastoma, Fibroma non-ossificans etc.
In the present case report, we have included a case of a non-aggressive CGCG endured by a young patient.
Case Report
A 11-year-old male reported to the OPD of the Department of Oral and Maxillofacial Surgery, Jaipur Dental College, Maharaj Vinayak Global University with an extensive firm and non-tender swelling on the front side of his mandible since 7 to 8 months, that was causing facial asymmetry. The patient gave non-contributory medical history. He had a history of extraction in the lower left posterior region 4-5 months back.
Clinical examination revealed an intra-oral reddish pink sessile lesion causing buccolingual expansion. The swelling was more prominent on the buccal aspect than the lingual aspect. (Figure 1)
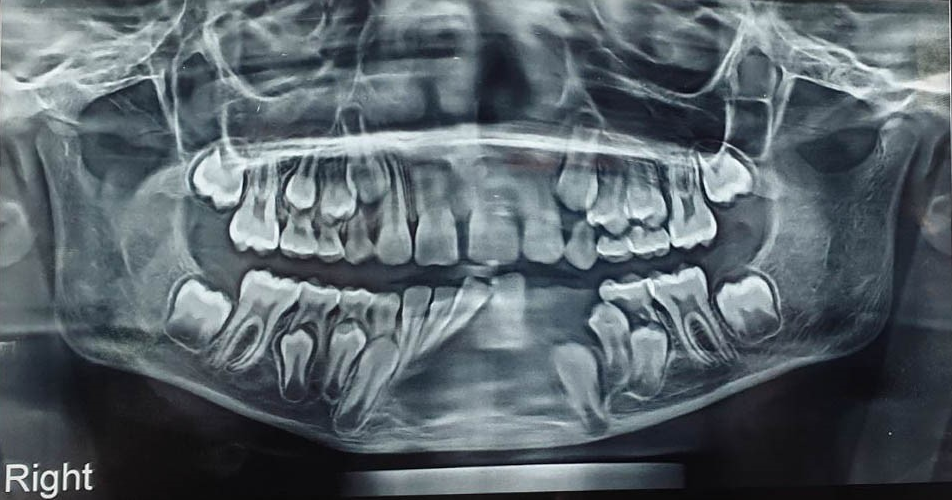
On the panoramic radiograph (OPG) an extensive multilocular radiolucency that extended from the distal aspect of lateral incisor of the right side till the distal aspect of the deciduous second molar on the left side crossing the midline. This lesion also displaced both central incisors and right lateral incisor towards the right side. (Figure 2)
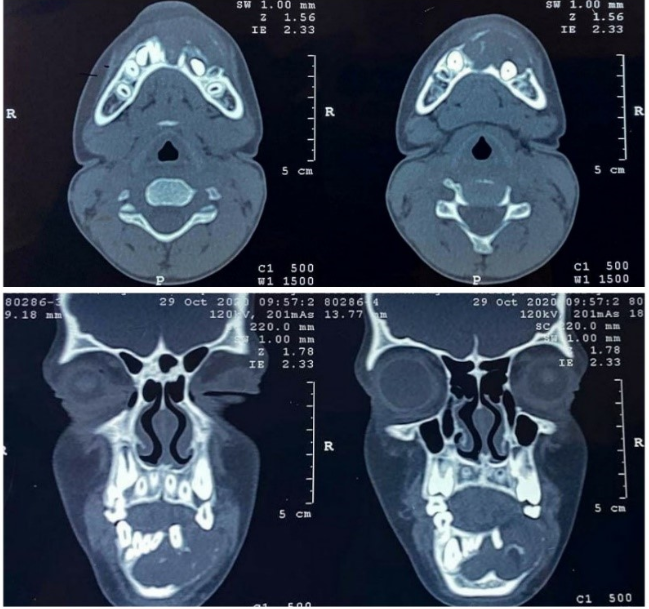
Specialized radiography with Computerised Tomography (CT) scan on axial section showed the lesion causing buccolingual expansion with perforation of the buccal cortical plate. On coronal section, it showed to be crossing the midline of the mandible extending till the inferior border. ($)
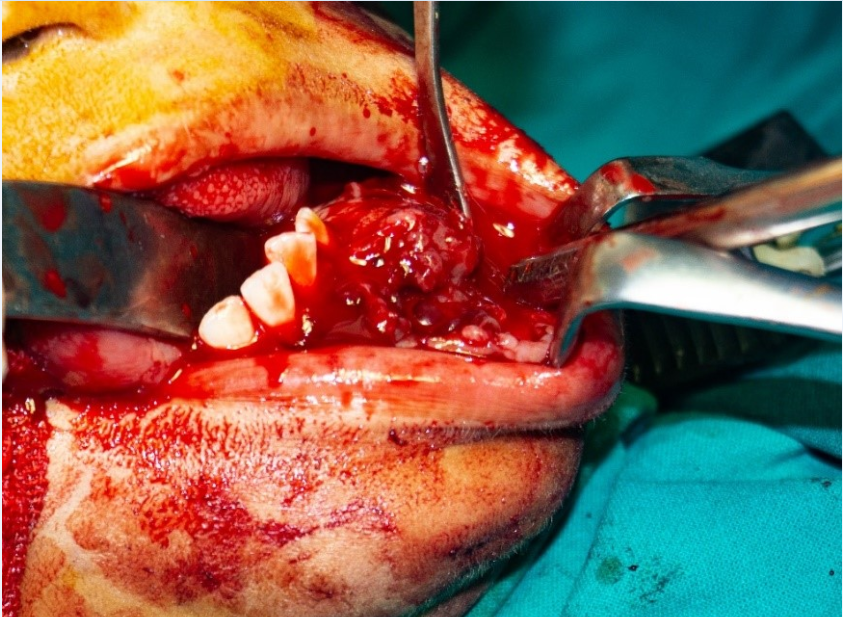
The blood investigations revealed that calcium (Ca), phosphorus (P) levels were normal. Parathyroid hormone (PTH) levels were elevated to122.6 pg/ml. Vitamin D supplementation was given to the patient regarding increased PTH and essential consent was obtained from endocrinologist after the PTH levels were normalized for the needful surgery. The patient was operated under general anaesthesia. The tumour mass was removed through an intraoral approach and curettage with peripheral ostectomy with preservation of the continuity of the mandible with at least a 5 mm margin was performed. (Figure 4)
Left central and lateral incisors and deciduous second molar were extracted. Right side central and lateral incisors were salvaged. The inferior alveolar nerve was preserved. Water tight closure was obtained with simple interrupted technique using 3-0 vicryl suture.
The lesion was sent for histopathological diagnosis. It was diagnosed to be a non-aggressive CGCG. The patient was followed-up for 1 year. He has not reported with any recurrence or any complication so far.
Discussion
This report describes a CGCG which invaded a broad portion of mandible which posed several local side effects and aesthetic and functional problems for the young individual. It was suggested that it might have been an inflammatory lesion, a reactive lesion, a true tumour, or an endocrine lesion.1, 8 On blood investigation and on opinion of our endocrinologist, we came up to a provisional diagnosis of non-aggressive CGCG. This required enucleation with peripheral ostectomy.
More than 70% of CGCGs occur in the mandible and less than 30% in the maxilla. Due to the special anatomical characteristics of the maxilla, its thin cortical plates allow the lesion to expand much earlier than in the mandible. Most lesions in the maxilla are in the anterior region, whereas in the mandible, the lesions seem to be more equally distributed anteriorly and posteriorly.8
CGCG usually presents as a painless swelling that remains undetected until facial asymmetry, impaired nasal breathing, loosening or displacement of teeth occurs. The lesion is expansile and invasive, however it does not violate the perineural sheets. For this reason, paraesthesia is not usually observed in such patients, as was the case with this patient.5
CGCG categorised into aggressive and nonaggressive types based on their clinical and radiographic characteristics. The more common, non-aggressive, lesions grow slowly and usually presented clinically as painless swellings, with only 20% of patients complaining of pain or paraesthesia.10 Radiographically they appeared as well-defined unilocular or multilocular radiolucencies with undulating borders. Aggressive lesions were encountered in a younger patient population and tended to grow faster and recur more often. The greater growth rate of these lesions was evident radiographically as ill-defined borders with variable amounts of cortical destruction.1
The principal treatment of CGCG is surgery.4 In this young patient, the lesion was successfully enucleated and curetted by an intra-oral approach which provided wide and quick access to the mandible with minimal post-operative sequelae and the best aesthetic results.
Pharmacological agents, are frequently used as alternative therapeutic modalities. Intralesional injections of steroids, calcitonin or systemic interferon alpha have shown encouraging Results. Interferon alpha is an antiangiogenic agent, which in combination with curettage, has proved successful in controlling tumour growth with decreased operative morbidity compared with conventional surgical treatment. Calcitonin is administrated either as nasal spray or in conjunction with injections, or as subcutaneous daily injections which cause reduction in tumour size but complete remissions were not observed. Patients have responded well to intralesional administration of triamcinolone acetonide. Successful application of this drug therapy in combination with curettage and peripheral ostectomy can prevent a mutilating procedure.3
The following lesions other than CGCG has been differentially diagnosed are giant cell lesions of bone: lesions of primary or secondary hyperparathyroidism, fibrous dysplasia, cherubism and aneurysmal bone cyst. Brown tumour which is secondary to hyperparathyroidism could be ruled out on the basis of normal serum levels of calcium, phosphorus, alkaline phosphatase and good renal function. Because the brown tumour is identical to CGCG histologically and radiographically, therefor it is essential to obtain blood investigations of every patient who has a giant cell lesion.5
Conclusion
Currently, no biological markers are known to predict clinical behaviour, and standard histological techniques are not helpful for the clinician to determine the prognosis. Surgery has always been considered to be the traditional treatment and it is still the most accepted. In surgery for large CGCGs the approach should be determined by both aesthetic outcomes and consideration of the possibility of excessive bleeding, which may require reserving blood prior to surgery. If soft tissues and periosteum are preserved, and only the bony component is excised, then it is possible to reconstruct the surgical defect with autogenous bone grafts. By doing this the bone continuity is maintained and prosthetic rehabilitation via implants can be safely performed.