Introduction
The influence of genetic and environmental factors in the etiology of dental malocclusion has been a debate and controversy in orthodontic literature.1 Malocclusions have a multi-factorial origin and can hardly be attributed to a single specific cause. The causes will include general factors, such as genetic and hereditary components, nutritional deficiencies, abnormal pressure habits and local factors located directly in the dental arch such as supernumerary teeth, tooth decay and premature loss of deciduous teeth.1 However, genetics plays a significant role in causing malocclusions. Epidemiological evaluations can reveal relationships between malocclusions and genetic characteristics or accompanied diseases, which will help to recognize and treat them. One of the most important human genetic characteristics is the relationship between the ABO blood group system and malocclusions.2 With the use of ABO blood groups and some enzyme polymorphs, it is be possible to determine the zygosity of twin, which are especially helpful in twin studies concerning the role of heritability of malocclusion.2
ABO blood group system is one of the most important system defined in 1901 by Karl Landsteiner who received a Nobel Prize in 1930 and together with Weiner, discovered Rh system in 1940.3 There are two antigens, A and B, in the ABO system, which are present on cell membranes or secreted into the plasma and other fluids of the body. The presence or absence of these antigens results in four blood groups or blood types: A, B, AB, and O. These antigens are present on the 9th chromosome and are inherited codominantly.4 Since the malocclusion and blood groups are related to genetic components, it can be hypothesized that blood groups have an association with dental malocclusions. Research has been carried out to find out the relationship between ABO blood groups and various systemic diseases, and the results showed that some diseases like dental caries,5 salivary gland tumors,6 oral cancer,7 hematological malignancies,8, 9 etc. have significant association with blood groups.
Weber et al. in 1927 conducted a study to find out the association of ABO blood groups with periodontal disease.10 Kaslick et al. conducted a study to find out the association of aggressive periodontitis and ABO blood groups, they found significantly less association of patients with blood group O and more association of patients with blood group B.11 Roberts et al.in his study concluded that the relationship between ABO blood group and susceptibility to chronic disease is an example of genetic basis for family predisposition.12 Koregol et al. in a study recorded that blood group A formed a significantly higher percentage in the gingivitis group, blood group O formed a higher percentage in the periodontitis group and blood group AB showed the least percentage of periodontal diseases.13
Not many studies have been conducted to determine the relationship between ABO blood groups and the incidence of oral diseases and malocclusion. Although the reports of some researchers claimed that there was a noticeable relationship, some others couldn’t find any relationship. Due to the lack of conclusive data on the relationship of blood groups with malocclusion, this study on the association of blood groups and malocclusion will be beneficial.
Materials and Methods
The sample of 132 subjects consisting of 56 males and 76 females from the department of orthodontics of our university for treatment of malocclusion. They were divided into Class I, Class II and Class III malocclusion as well as horizontal and vertical skeletal patterns.
Cephalometric analysis was carried out using lateral cephalogram. Parameters for cephalometric analysis was 3 sagittal skeletal parameters and 3 vertical parameters. 3 sagittal parameters included were ANB, YEN angle and Beta angle. 3 vertical parameters included were FMA, SN-GoGn and Y axis. Two parameters should be positive for categorizing the subject into vertical and sagittal. Patients blood group was analyzed using slide method and divided as ABO and Rh blood groups. Results were correlated with malocclusion to find out the relationship between blood group and malocclusion.
Sagittal dental parameters
Dental parameters were analyzed and categorized according to Angle’s classification of malocclusion, i.e. Class I, Class II and Class III malocclusions.14
Class I Malocclusion
Angle’s Class I molar relationship is one in which mesio-buccal cusp of maxillary first permanent molar occludes in the buccal groove of mandibular first permanent molar with one or more of these characteristics: Crowded incisors or labial canines, protruded maxillary incisors, anterior end to end occlusion or anterior cross bite, unilateral or bilateral posterior cross bite, mesial drift of molars, anterior or posterior open bite and deep anterior overbite.14
Class II Malocclusion
Angle’s Class II molar relationship is one in which disto-buccal cusp of maxillary first permanent molar occludes in the buccal groove of mandibular first permanent molar with proclined maxillary incisors and increased overjet (Angles Class II div 1 malocclusion) or with retroclined maxillary central incisors and proclined lateral incisors (Angles Class II Div 2 malocclusion).14
Class III Malocclusion
Angle’s Class III molar relationship is one in which mesio-buccal cusp of maxillary first permanent molar occludes in the inter-dental space between mandibular first and second permanent molars with end to end incisor relationship or with normal incisor relationship with incisors in cross bite relationship. 14
Sagittal skeletal parameters
Skeletal patterns were analyzed and divided into Class I, Class II and Class III using the following parameters
YEN Angle
Is formed by the intersection of S (Sella), M (midpoint of the anterior maxilla), and G (center at the bottom of the symphysis), to form the YEN angle measured at M (117-1230)
ANB Angle
It is the angle between SNA and SNB consist of A point, Nasion, B point and indicates whether the skeletal relationship between the maxilla and mandible is a normal skeletal class I (+20), a skeletal Class II (+40 or more), or skeletal class III (00 or negative) relationship.
Beta Angle
The angle between the A-B line and the perpendicular through point A from the apparent axis of the condyle (C) constitutes the beta angle. Beta angle between 270- 350 can be considered to have class I skeletal pattern.
Vertical skeletal parameter’s
Skeletal patterns were analyzed and divided vertical, horizontal and average using the following parameters
FMA
It is the angle formed between the Frankfort horizontal plane (FH) and the mandibular plane. FMA of 250+/- 50 is within normal range. A high angle patient has an FMA of 300 or more, and a low angle patient has FMA of 200 or less
SN- Go Gn Angle
According to Steiner SN- GoGn is formed by the intersection of mandibular plane (Go-Gn) and Sella (S) and Nasion (N) Larger angle indicate a vertical facial pattern, low angle indicates horizontal facial pattern, the mean angle is 320 in average facial pattern.
Y-Axis
Down's analysis uses Y- axis to assess the vertical skeletal discrepancies. This angle is formed at the intersection of Sella-Gnathion line with the Frankfort Horizontal Plane. Larger angles indicate vertical facial patterns, and low angles indicate horizontal facial patterns, the mean angle is 59.40 in average facial patterns.
Blood Grouping or Blood Typing
The surface of red cell membrane contains a variety of genetically determined antigens, called isoantigens or agglutinogens while the plasma contains antibodies (agglutinins). To determine the blood group of a person, his/her red cells are made to react with commercially available antiserum containing known agglutinins. The slide is then examined by naked eye or under the microscope to detect the presence or absence of clumping and hemolysis (agglutination) of red cells, which occur as a result of antigen-antibody reaction.
Specimen collection and processing
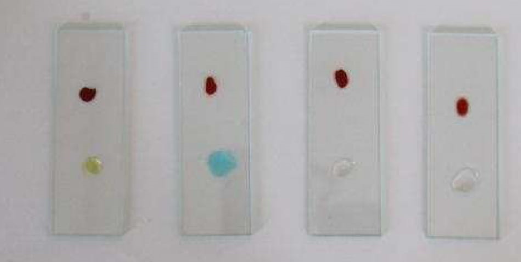
A microscope, a glass dropper with a long nozzle, sterile blood lancet or needle, sterile cotton or gauze swabs, alcohol, toothpicks, clean and dry microscope slides, 1% sodium citrate in normal saline, anti-A serum (also called anti-A or alpha agglutinins), anti-B serum (anti-B or beta agglutinins) and anti-D or anti Rh serum were used. For quick identification, the anti-A serum is tinted blue; anti-B is tinted yellow and anti-D is colorless (Figure 1).
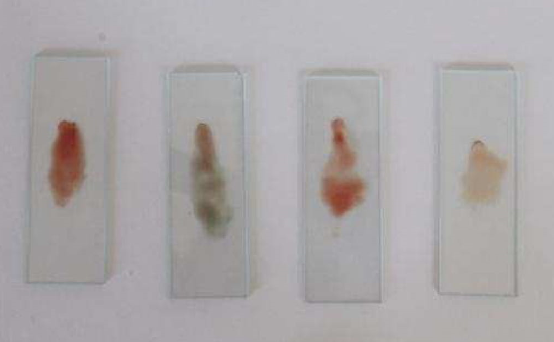
Based on standard lab procedure, 4 slides were used. One slide was marked with anti-A, other marked anti-B and the third slide was marked anti-D, fourth slide was marked C for red cell suspension in saline. No antiserum was added to this (Figure 2).
Finger was pricked under aseptic conditions and two drops of blood were added to the saline on the slide and mixed with toothpick to prepare red cell suspension.1 drop of antisera A, B and D was placed on the respective slides and 1 drop of normal saline was placed on control slide to confirm agglutination or no agglutination.(Figure 2) Antisera and red cell suspension were mixed with the help of separate toothpicks. After 8-10 min, all the three antisera- red cell mixtures on the slide were inspected, first with the naked eye to see whether agglutination (clumping or hemolysis) had taken place or not and using the control slide as reference. (Figure 3). Agglutination appeared as a coarse separation of red cells in isolated clumps (red precipitates of cells) and this agglutination was confirmed under low magnification microscope.
Thus, the presence or absence of agglutination indicated the individual’s blood group or blood type as A, B, AB and O along with Rh+ve and Rh-ve (Table 1).
The cephalometric values were measured, tabulated, analyzed and classified according to dental, sagittal and vertical using Angles classification of malocclusion (Table 2, Table 3), ANB, YEN angle Beta angle, Y-Axis, SN -GoGn and FMA
The data collected was statistical analyzed and the information obtained was processed using SPSS software (version 20) and the Chi-square test (Table 4). Kruskal Wallis test and Mann Whitney U test (Table 5) were performed to compare significant differences in each testing parameters with blood groups. The differences with P < 0.05 were considered statistically significant
Results
This study was conducted to assess correlation between blood groups with different dental and skeletal parameters. Statistical analysis of 132 participants, showed that there is a significant difference in relationship between blood group and sagittal skeletal parameters particularly YEN angle. There is no association of blood groups with dental, vertical skeletal parameters and other sagittal skeletal parameters, Chi- square test showed no association of blood groups with different dental and skeletal parameters. The Kruskal Wallis test revealed that there is statistically significant difference in parameters between the different blood groups. There was a significant difference in YEN angle across the blood groups. The Kruskal Wallis against SN-GoGn with blood group showed that there is no significant difference in SN-GoGn between different blood groups (Table 6) but which pair median differ significantly was not known so a post Hoc comparison was performed Mann Whitney U test showed that there is a significant difference in Yen angle between B and O blood groups (Table 6).
Table 1
Blood typing reference chart
|
Blood group |
Antiserum A |
Antiserum B |
Antiserum D |
|
A/A- |
+ |
- |
+/- |
|
B/B+ |
- |
+ |
+/- |
|
O/0- |
- |
- |
+/- |
|
AB+/AB- |
+ |
- |
+/- |
Table 2
Distribution of malocclusion per each blood group
|
Blood groups |
Malocclusions |
Total (132) |
Total in % |
||
|
Class I (79) |
Class II (44) |
Class III (9) |
|||
|
A |
16 |
9 |
2 |
27 |
20.45 |
|
B |
22 |
14 |
2 |
38 |
28.7 |
|
AB |
4 |
2 |
3 |
9 |
6.81 |
|
O |
37 |
19 |
2 |
58 |
43.93 |
Table 3
Malocclusion cross table.
Table 4
Chi-square Test.
|
|
|||||
|
|
Value |
Df |
Asymp. Sig. (2-sided) |
P value |
|
|
Pearson Chi-Square |
11.408a |
6 |
.077 |
.075 |
|
|
|
|
|
|
|
|
Table 5
Kruskal Wallis Test
|
Parameters |
Chi-Square |
P Value |
|
Yen angle -Sagittal growth parameter |
14.655 |
0.002 |
|
SN-GoGn – Vertical growth parameter |
1.562 |
.668 |
Table 6
Post Hoc test mann-whitney (Yen angle sagittal growth parameter)
Discussion
This study on the association between malocclusion and blood groups, included subjects who were clinically assessed by a single operator to minimize inter-operator bias. Subjects with overall good health were included to assess blood groups, so as to have a proper evaluation and classification of blood groups. The distribution of ABO blood groups may also vary regionally, and from one population to another. Malocclusion is a multi-factorial disease and the etiology of the disease has not been clearly established yet with genetic factors probably playing a role. The purpose of this study was to identify such a possibility and to correlate blood group and with malocclusion
During the last few years, several reports have suggested that ABO blood groups, specifically.
Non O blood groups are associated with the risk of ischemic heart disease and of developing severe manifestations of atherosclerosis. 8, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 Compared to A, B and AB individuals, O group individuals have a 14% reduced risk of squamous cell carcinoma and 4% reduced risk of basal cell carcinoma and pancreatic cancer. 26 The B antigen has linked with increased risk of ovarian cancer Gastric cancer has been reported to be common in blood group A and least in group O According to Glass et al. 9 the O blood group has an increased risk of infection with cholera and the severity of infection was worse compared to others. Reid et al. 17 and Hadley et al. 18 have shown relationship between blood group and congenital cataract in the Asian race. Cardiovascular diseases are more prevalent in A, O and non-O blood groups. 5, 17, 19, 20 Diabetes mellitus may be higher in subjects of blood groups A and O. 21 Along with these findings, the ABO groups have been suspected of having a role in causation of infertility and fetal loss, but reports were found to be conflicting. 22
Thus, it is clear that several studies have been carried out to investigate the relationship between ABO blood group and incidence of disease in medicine, but limited research has been carried out to investigate the association between ABO blood groups and oral diseases. Few reports claimed that there was a relation of blood groups and increased incidence of oral diseases. 5, 13, 23, 24, 25, 27, 28 However some others could not find association, which may be due to geographical diversity in the population. 11, 23, 24, 25, 29, 27 Vivek et al. 27 found that subjects with blood group O and Rh+ had a greater propensity for periodontitis . Gheisari et al. 30 showed that among different blood groups; blood group B were found to have a greater association with other dental malocclusion and the association of such deformities was found to be the least with blood group A. Demir et al.28 found that different ABO blood groups show significant differences in the rates of colonization of periodontal pathogens that are the main etiologic agents of periodontal diseases. It has also been reported that blood group A seems to have an association with oral pathologies such as dermatophytosis. 31
In this study of the evaluation of the association between blood group and dental malocclusion reveals that blood groups have an association with dental malocclusion. Relationship of blood groups with malocclusion is statistically significant (p< 0.0001), indicating the prevalence of malocclusions. The post Hoc test result shows that there is significant difference in YEN angle between B and O blood groups. The Kruskal Wallis test showed that there is no significant difference in SN-GoGn between different blood groups.