- Visibility 200 Views
- Downloads 30 Downloads
- Permissions
- DOI 10.18231/j.idjsr.2021.008
-
CrossMark
- Citation
Treacher collins syndrome- A case report
- Author Details:
-
Vinod Sankar
-
Arun George
-
Atic Thomas
-
Leyons Augustine *
Abstract
Treacher Collins syndrome (TCS), mandibulofacial dysostosis, or Franceschetti–Zwahlen–Klein syndrome, is a rare genetic disorder characterised by dysgenesis of the hard and soft tissues of first and second branchial arches. Bimaxillary surgery can improve the maxillomandibular facial projection. In this article we shows maxillofacial management of 23 year old male with Treacher Collins Syndrome.
Introduction
Treacher Collins syndrome (TCS) was named 96 years after the British ophthalmologist Edward Treacher Collins who described the condition in 1900. Franceschetti and Klein, who extensively reviewed the essential components of the condition, used the term Mandibulofacial dysostosis to describe the clinical features. It is described as an anomaly of the first and second pharyngeal arch, it can extend to the cervical spine. [1]
Epidemiology
An autosomal dominant condition, mainly affecting those parts derived from the first and second branchial arches.It occurs at a frequency of 1 in 25,000 to 1in 50,000 live births. [2]
Genetics
Treacher Collins syndrome is caused by mutations in the TCOF1 gene. TCOF1 was mapped to chromosome bands 5q31.3-33.3. The TCOF1 gene codes for the treacle protein, which may be involved in nucleolar trafficking and is required for normal craniofacial development. 60% cases occur as a result of fresh mutation. [2]
Oral and Craniofacial features
Mandibular retrognathia is the defining feature of TCS. Fish –like or Bird-like face with Dolichofacial pattern, down-slanting eyes (“crying facies”), hypoplastic supraorbital rims, hypoplastic zygoma, processes of hair that extend towards cheek. Dorsal nasal hump with conductive hear loss, notched upper or lower eyelids with hypertelorism are the typical facial features. [3], [4] Facial features are bilateral and symmetrical. Parotid gland hypoplasia or aplasia are also seen. There are multiple oral manifestations of TCS. Examples include high palatal vault, clefting of the palate, and enamel hypoplasia. Skeletal hypoplasia of the maxilla and mandible often leads to an anterior open bite. [5]
Case Report
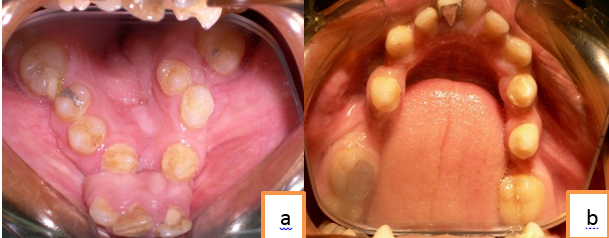
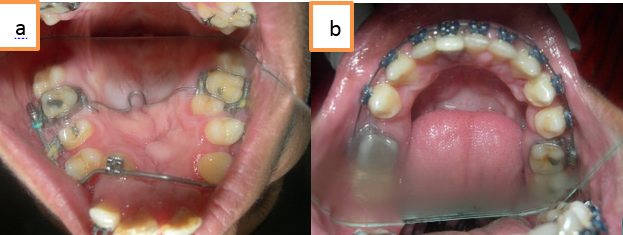
A 23 year old male reported to the department of oral and maxillofacial surgery at Mar Baselios Dental college, Kothamangalam with a chief complaint of crooked teeth, with a positive medical history coinciding with TCS. The extra oral examination showed right microtia,([Figure 2]), malar hypoplasia, micrognathia, convex profile, and severe lip incompetence ([Figure 1]). The intraoral examination revealed anterior and posterior crossbite with reverse overjet of 5mm ([Figure 4]). His maxillary arch was severly constricted with malpositioned tooth. Severe arch length tooth size discrepancy was also noted.



Treatment objectives
The treatment objectives for this patient required both orthodontic and surgical treatment, including correction of the maxillary transverse discrepancy, elimination of dental crowding, correction of the cross bite, establishment of overbite and overjet for proper function, and improvement of the soft-tissue profile.
Treatment plan
The treatments initially focus on presurgical Orthodontics, for correction of malaligned teeth. First Surgical Phase of management includes Mandibular Subapical osteotomy with Upper lip repair including Columellar lengthening and Alar base shortening. Constricted maxillary arch can be managed with expansion of the Upper arch using Bandelette Appliance. Second surgical phase includes Bilateral Sagittal Split Osteotomy (BSSO) setback with Genioplasty advancement to correct chin deficiency. Prosthetic reconstruction of ear can be considered after surgical phase Post Surgical Orthodontic correction can be carried out finally. [6]
Treatment progress
Pre surgical orthodontics begins with fixed orthodontic treatment and Bandelette Appliance used for expansion of maxillary arches, and also combined with maxillomandibular arch wires for alignment of teeth.([Figure 5]). Anterior crossbite correction has been done after initial leveling and alignment with Lower sub apical osteotomy and achieved proper anterior overjet ([Figure 3]). After presurgical orthodontics patient had undergone following procedures, Upper lip repair by Columellar lengthening and Alar base shortening, Bilateral sagittal split osteotomy set back ([Figure 6], [Figure 7] ). Prosthetic reconstruction of ear.([Figure 3]). Postsurgically, the patient continued with the finishing stages of orthodontic treatment in light round wires. Upon debonding of the fixed appliances, he was given retention appliance.


Discussion
TCS is a disorder of congenital type which significantly affects craniofacial development. Some patients show severe deformation while others posses only mild changes. Our patient shows significant changes like microtia, malar hypoplasia, micrognathia, convex profile, and severe lip incompetence. Correction of bilateral cleft lip has been undergone during early childhood Management of TCS is a multidisciplinary approach, which include several consultants from medical and dental specialities like craniofacial, maxillofacial plastic surgeons, orthodontists and dentists (paediatric or restorative).
Posnick et al has showed the efficacy of reconstructing malar and orbital deficiencies using a full thickness calvarial bone graft. Recent advances in synthetic biocompatible materials such as high-density polyethylene (Medpor, Stryker Corporation, Kalamazoo, USA) have provided new possibilities in hard tissue augmentation.[5] Mulliken et al described the principles of surgical reconstruction of the bilateral cleft lip. According to him maintenance of symmetry, securing primary muscular union, correct design of the prolabial flap, formation of the median tubercle and the vermillion- cutaneous ridge by tissue from the lateral segments.[7] Chigurupati et al shows bilateral sagittal split mandibular osteotomy horizontally retracts the mandible, closing the anterior crossbite, which can be combined with a sliding genioplasty to correct retrogenia.[8] While looking to external ear reconstruction According to Brent reconstruction can be successfully carried out by rib cartilage taken from side controlateral to ear which is reconstructed.[9] Ear reconstruction using osseointegrated implants can provide good esthetic results, but limits usage as it can result in chronic irritation.[10], [11] In our case we carried out with BSSO set back with maxillary arch expansion using rapid expansion appliance. Finally microtia corrected with prosthetic ear. Postoperative lateral cephalogram shows significant improvement in skeletal anatomy.
Conclusions
The current approach to treat TCS is to stage reconstruction which should correlate with growth pattern. Coordinated care with early diagnosis by craniomaxillofacial team can provide optimal results. The functional and aesthetic desires of each person with TCS is different ,so anyhow a general scheme of approach can only be carried out.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- Chung J, Cangialosi T, Eisig S. Treacher Collins syndrome: A case study. Am J Orthod Dentofac Orthop. 2014;146(5):665-72. [Google Scholar] [Crossref]
- Cobb A, Green B, Gill D, Ayliffe P, Lloyd T, Bulstrode N. The surgical management of Treacher Collins syndrome. Br J Oral Maxillofac Surg. 2014;52(7):581-9. [Google Scholar] [Crossref]
- Caccamese J, Ruiz R, Costello B. Costochondral Rib Grafting. Atlas Oral Maxillofac Surg Clin. 2005;13(2):139-49. [Google Scholar] [Crossref]
- Kline RM, Wolfe SA. Complications Associated with the Harvesting of Cranial Bone Grafts. Plastic and Reconstructive Surgery. 1995;95:5-13. [Google Scholar] [Crossref]
- Posnick J, Tiwana P, Costello B. Treacher Collins syndrome: comprehensive evaluation and treatment. Oral Maxillofac Surg Clin North Am. 2004;16(4):503-23. [Google Scholar] [Crossref]
- Thompson JT, Anderson PJ, David DJ. Treacher Collins syndrome: protocol management from birth to maturity. J Craniofac Surg. 2009;20(6):2028-35. [Google Scholar]
- Mulliken J. Repair of bilateral cleft lip and its variants. Indian J Plast Surg. 2009;42. [Google Scholar] [Crossref]
- Chigurupati R. Orthognathic Surgery for Secondary Cleft and Craniofacial Deformities. Oral Maxillofac Surg Clin North Am. 2005;17(4):503-17. [Google Scholar] [Crossref]
- Brent B. Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstru Surg. 1992;90(3):355-74. [Google Scholar]
- Firmin F. State-of-the-art autogenous ear reconstruction in cases of microtia. Aesthetics Functionality Ear Reconstr. ;68:25-52. [Google Scholar]
- SN, Gül EB, MG. Bilateral implant-retained auricular prosthesis in a patient with Treacher Collins syndrome: a case report. Acta Odontologica Turcica. 2014;31(1):31-5. [Google Scholar]
How to Cite This Article
Vancouver
Sankar V, George A, Thomas A, Augustine L. Treacher collins syndrome- A case report [Internet]. Int Dent J Stud Res. 2021 [cited 2025 Oct 30];9(1):39-42. Available from: https://doi.org/10.18231/j.idjsr.2021.008
APA
Sankar, V., George, A., Thomas, A., Augustine, L. (2021). Treacher collins syndrome- A case report. Int Dent J Stud Res, 9(1), 39-42. https://doi.org/10.18231/j.idjsr.2021.008
MLA
Sankar, Vinod, George, Arun, Thomas, Atic, Augustine, Leyons. "Treacher collins syndrome- A case report." Int Dent J Stud Res, vol. 9, no. 1, 2021, pp. 39-42. https://doi.org/10.18231/j.idjsr.2021.008
Chicago
Sankar, V., George, A., Thomas, A., Augustine, L.. "Treacher collins syndrome- A case report." Int Dent J Stud Res 9, no. 1 (2021): 39-42. https://doi.org/10.18231/j.idjsr.2021.008
