Introduction
Alveolar ridge resorption is an inevitable phenomenon observed following the removal of teeth in an otherwise healthy individual. The condition appears to be progressive and irreversible, resulting in a host of prosthodontic, aesthetic, and functional problems. Post extraction bone loss is accelerated in the first 6 months, followed by a gradual modelling (change in size or shape) and remodeling (turnover of existing bone) of the remaining bone, with as much as In the first 6 months, 40 percent alveolar height and 60 percent alveolar width were lost.1 Loss of ridge height results in prosthetic instability as the crest of the ridge approaches muscle attachments and mobile mucosa. In extreme cases, there may be involvement of the maxillary sinus or nasal cavity, requiring extensive reconstructive surgery for traditional or implant-supported prosthetics.
Vital structures can become susceptible, such as the mandibular neurovascular bundle due to exposure and Overlying impingement of the denture. 2 Bone loss occurs generally on the horizontal plane at the expense of the buccal or facial bone. A number of clinical studies have shown that dimensional changes and significant alterations occurs in post extraction ridge. Atwood, 1963; 3 Schropp and colleagues, 2003; 4 Araujo & Lindhe, 2005. 5
The Osteology Consensus group conference reported that, after extraction, the average ridge width loss was 3.8mm and average ridge height loss was 1.24mm. Reviews by Hammerle et al 2012,6 Pelegrine et al 2012,7 Tan, Wong et al. 20128 also validated the same.
The aesthetic and functional outcomes of dental implant therapy are highly dependent on sufficient alveolar bone volume following tooth extraction. Although bone loss prior to extraction may have occurred due to trauma, periapical pathosis, or periodontal disease; it is important to understand that alveolar ridge bone loss occurs after extraction. In the normal post extraction remodeling process, without an intervention to preserve alveolar ridge contours, bone loss occurs in both horizontal and vertical dimensions. 3 Considering that the dimensions of the alveolar ridge are critical for implant placement, it is imperative to recognize that site (ridge) preservation following tooth extraction is needed to maintain as ideal an alveolar ridge anatomy as possible.
Hydroxyapatite (HA) and Beta-Tricalcium Phosphate (β-TCP) used in this study is an osteoconductive biphasic calcium phosphate (β-TCP) with higher i.e. seventy per-cent and thirty percent HA thus, the availability is in abundance and there are no chances of antigenic response (dis-ease transfer) towards a foreign body. It has been used in regenerative therapies but the possible additional benefit laser curettage at extraction site in promoting new bone formation has not been previously evaluated histologically in a twelve week of time interval.
Material and Methods
The study was conducted in Department of Prosthodontics and Crown & Bridge and Oral Implantology, Manav Rachna Dental College, Faridabad, India. The ethical committee (MRDC/IEC/2017/11) approved the study protocol, and informed consent form. Patients were selected with teeth having poor prognosis and indicated for extraction to participate in the study. Eligibility criteria were posterior tooth (molar or premolar) scheduled for extraction and implant placement; subjects aged ≥ 18 years-65 years; systemically and periodontally healthy; non-smoker; able and willing to comply with study procedures and multiple visits. Exit criteria were voluntary withdrawal; non-compliance with study procedures; development of systemic or oral diseases; subjects requiring surgical protocol modification (e.g. indication for Guided bone Regeneration procedure).
separated with a diamond bur, atraumatic extraction was performed using periotomes and luxators, socket debridement was performed with the aid of curette and saline irrigation (Figure 2).
Table 1
Demographic details of the study population
|
Variables |
|
|
|
Age (n=20) |
Mean |
Range |
|
|
34.30 |
18-48 |
|
Age Groups |
n |
|
|
≤35 Years |
10 |
|
|
>35 Years |
10 |
|
|
Sex |
n |
|
|
Male |
14 |
|
|
Female |
6 |
|
The socket curetted was followed by application of laser diode (Biolase Epic x) for 30 seconds (for indicated number of cycles) at 0.8w (Figure 3). Flaps were released, to achieve primary closure whenever possible. Then, alloplast graft (OsteonII Dentium, -Korea) (Figure 4). (a combi-nation of particle size 02-0.5 mm and 05.-1.0 mm) and collagen membrane (Periocol) was stabilized in the buccal flap and sutured (Ethicon Vicryl 5-0). After 1 week, the wounds were cleaned with saline irrigation and visually inspected. Socket preserved sites were scheduled for implant surgery after 12 weeks’ time interval. Augmented sites were re-entered via a crestal incision that was connected with sulcular incisions on the neighboring teeth. At re-entry, a standard drilling technique was utilized except for a modification in the depth of the osteotomy with a trephine drill (Norris (2 mm inner diameter and length 8mm), and biopsy obtained from study sites. Copious sterile saline was used during osseous drilling procedure cylindrical bone cores (average diameter = 2 mm, length = 8 mm) (Figure 7) were obtained and then the osteotomy was increased with progressive drills to the appropriate size, based on final implant dimensions. Before histological preparation, the cylindrical cores harvested were marked with blue ink at the coronal side to identify the coronal and apical region. Specimens obtained from the grafted areas were fixed in 10% formalin then decalcified in 10% nitric acid.
Paraffin embedding was done and 4 micrometer thick sections were prepared and stained with Hematoxylin– Eosin and Masson’s trichrome. For the qualitative ana-lysis of the remodeling process, the stained preparations were examined under a light microscope at a magnification of up to 10(X) and 40(X). Two regions of interest (ROI) the apical and the coronal portion were analyzed. In each ROI the amount of lamellar bone, woven bone and connective tissue were calculated with the aid of an imaging software Magnus Pro 4.2.
Results
Healed extraction sockets were evaluated after 12 weeks ± 4 days of healing period.
Histological evaluation
It was performed to evaluate the bone formation and various tissue components. It was found that was 34.30 ± 8.58 mean percentage of lamellar bone formation, 23.72 ± 6.96 mean percentage of woven bone formation and 39.81 ± 5.97 mean per-centage of connective bone formation occurred.
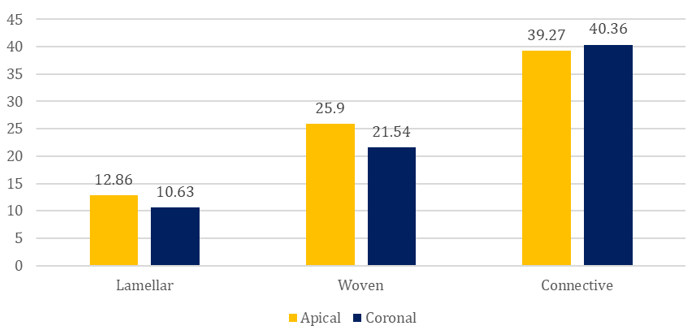
The comparison of mean percentage of new bone formation between the apical and coronal part of bone core was done. It was found that statistically significant (p=0.035) difference was found in mean per-centage of new lamellar bone formation between apical and coronal part of bone core. The mean per-centage of new lamellar bone formation at apical part (12.86 ± 2.81) of bone core was higher than the coronal part (10.63 ± 3.88).
Statistically significant (p=0.035) difference was also found in mean per-centage of new woven bone formation between apical and coronal part of bone core. The mean percentage of new woven bone formation at apical part (25.90 ± 6.71) of bone core was higher than the coronal part (21.54 ± 6.64). No statistically significant (p=0.551) difference was found in mean percentage of new connective bone formation between apical and coronal part of bone core. However no statistically significant difference was found in mean percentage of new lamellar (p=0.141), woven (p=0.349) and connective (p=0.829) bone formation between apical and coronal part of bone core in the maxilla was seen.
The comparison of mean percentage of new bone formation between the age groups was done. It was found that highly statistically significant (<0.001) difference was found in mean percentage of new woven bone formation between ≤ 35-years and > 35-year age group was seen. The mean percentage of new woven bone formation of ≤ 35-years age group (27.00 ± 6.46) was higher than the > 35-year age group (19.80 ± 5.41). No statistically significant difference was found in mean percentage of new lamellar (p=0.148) and connective (p=0.284) bone formation between ≤ 35-years and > 35-year age group was seen.
Discussion
A plethora of bone graft materials have been utilized in the past two decades for socket preservation at the extraction site. Auto-graft being the gold standard for any augmentation procedure has a few disadvantages of creating donor site morbidity and limited graft size. Amount of bone fill, residual scaffold and connective tissue differ among studies and depend on various parameters: surgical procedure, material that was used to fill the socket, utilization of a membrane and healing period.
There are conflicting views with few authors regarding the use of grafting material for ridge preservation as an effective technique in repressing alveolar ridge resorption Barone 2012; 9 Iasella 2003,10 On the other hand few authors also argue that intrasocket grafts may compromise the physiological healing process of the extraction socket, or be of no advantage.
This phenomenon of bone formation was more pronounced in the apical portion which may indicate importance of proximity between the socket walls and the volume of the wound in that region might be critical factors in new bone formation. Greater accelerated bone regeneration in the apical portion of the socket has also been a consistent finding in previous studies. 11, 12, 13, 14
Figure 9
Histological section at apical portion(a) Masson’s Trichrome (MT) staining showing woven bone, lamellar bone in dense connective stroma at 4(x) magnification, (b) MT staining showing woven bone, lamellar bone in dense connective tissue stroma at 40(x) magnification. (c) Hematoxylin and eosinophilic staining showing bone within connective tissue stroma

Conclusion
The present study was a clinical interventional in nature. The aim of the current study was to histologically evaluate the bone in the augmented extraction socket over a period of twelve weeks. Within the limitations it was observed that the apical part of the socket showed higher bone formation than the coronal, also younger population were presented with a greater bone formation. There was no significant difference between the gender in bone formation. However, mandible also represented with greater bone formation than maxilla. It can be elucidated that all oplast can be held effective osteoconductive material for extraction socket augmentation.