Introduction
Physiological conditions such as puberty, pregnancy, menopause have significant effect on oral health of women. Hormonal changes during pregnancy have severe effects and consequences upon oral tissues. Most of its effects are visible on gingival tissues.1 immunological, dietary and behavioral factors associated with pregnancy are believed to be contributing factors. Increased levels of estrogen and progesterone in pregnancy can induce edema, hyperemia and bleeding in periodontal tissue as well as an increased chance for gingival enlargement. 2
Poor oral hygiene during pregnancy can lead to gingival and periodontal disease. In addition, they may not show symptoms until advance diseased disease stage and the prenatal risk increases unknowingly. This dependence is not only limited to preterm babies but also to adverse pregnancy results, loss of pregnancy or spontaneous abortion, stillbirth, toxemia, fetal growth restriction, premature birth, pre-eclapsia, ulcerations of the gingival tissues, pregnancy granuloma and tooth erosion. 3, 4, 5
The oral awareness and habits among the low socioeconomic people is still less. Targeting to improve pregnant women’s awareness of oral hygiene, can improve the oral health of her children and if lack of awareness is present, proper awareness program can be planned for pregnant women. Against this background, this survey is to be conducted to evaluate the oral health awareness and practices in pregnant women.
Materials and Methods
Participants included in the cross-sectional survey were pregnant females attending the OPD in the General Hospital, Muvattupuzha, Kerala. A total of 100 women were included in this study. Patients who were willing to participate in the study, was selected. Physically handicapped and patients with systemic problems were excluded from the study. A written informed consent was obtained from the hospital medical superintendent and also from pregnant women for conducting the study. A self-constructed questionnaire, containing 10 questions in English was explained and thus procured data was filled by the dental professional. Convenient sampling method was used. This study was reviewed and approved by the institutional ethics committee. Collected data was statistically analyzed.
Results
Sociodemographic characteristics
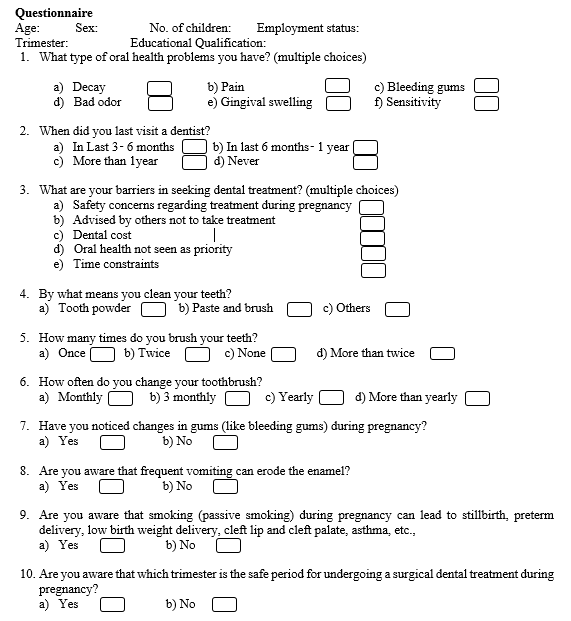
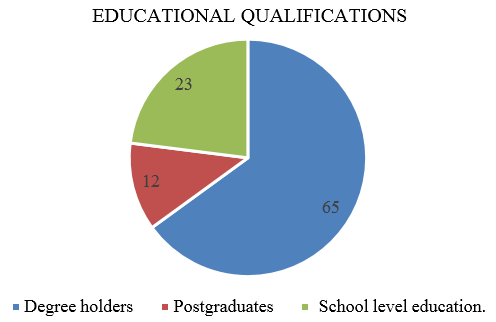
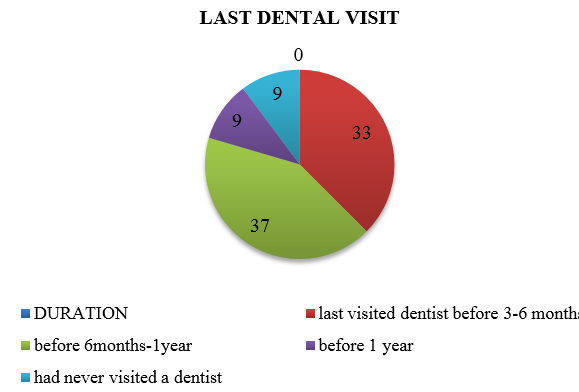
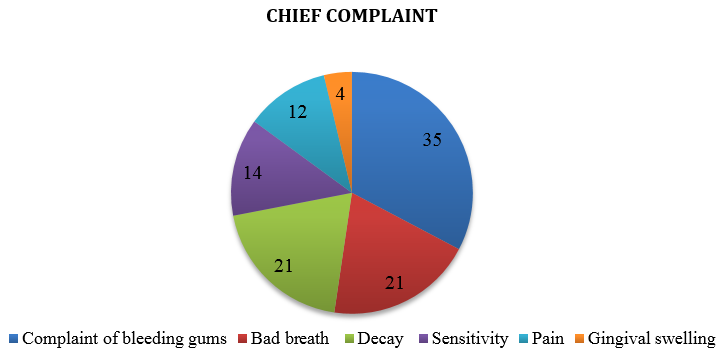
82% of total participants in the study were in the age group of ≤ 30. 51% of participants were housewives. 43% were in their first trimester, 36% in second trimester and 21% in their third trimester. 65% were degree holders, 12% were postgraduates and 23% had school level education. 35% had complaints of bleeding gums, 21% had bad breath and 21% had decay. 14% had sensitivity, 12% had pain and 4% had gingival swelling. 33% of participants had last visited dentist before 3-6 months, 37% before 6 months-1year, 9% before 1 year, and 9% had never visited a dentist.
Oral health practice
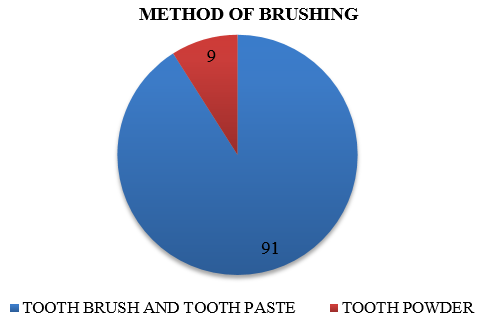
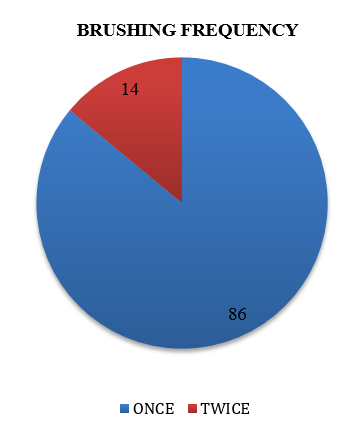
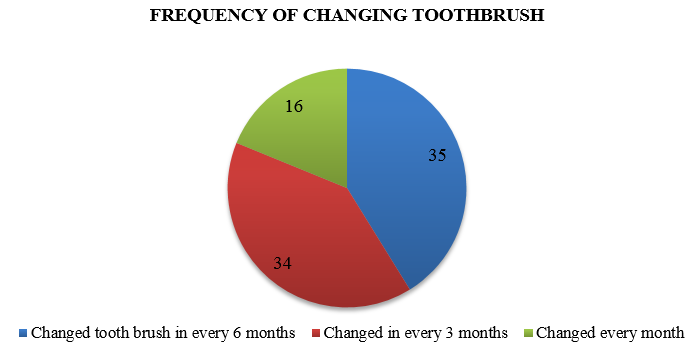
31% had not considered oral health as priority, 22% had safety concerns regarding treatment during pregnancy, 24% considered dental treatment cost as barrier in seeking dental treatment, 19% had time constraints, and 16% were advised by others not to take treatment. 91% used paste and brush as means of cleaning teeth, while 9% used tooth powder. 86% brushed only once per day, while 14% brushed twice daily. 35% changed tooth brush in every 6 months, 34% changed in every 3 months, and 16% changed every month. 32% had changes in gums (like bleeding gums) during pregnancy.
22% knew that frequent vomiting can erode the enamel. 69% were aware of the fact that smoking (passive smoking) during pregnancy can lead to stillbirth, preterm delivery, low birth weight delivery, cleft lip and cleft palate, asthma, etc., 22% were aware of which trimester was the safe period for undergoing a surgical dental treatment during pregnancy. 22 participants who had school level education, 55 participants who were degree holders and 9 participants who were postgraduates brushed once daily. 1 participant who had school level education, 10 participants who were degree holders and 3 participants who were postgraduates brushed twice daily.
Table 1
Table 2
Participants in each trimesters
|
|
Number |
Percentage |
|
First Trimester |
43 |
43.0 |
|
Second Trimester |
36 |
36.0 |
|
Third Trimester |
21 |
21.0 |
Table 3
Educational qualifications of participants
|
|
Number |
Percentage |
|
Degree |
65 |
65.0 |
|
postgraduate |
12 |
12.0 |
|
school level |
23 |
23.0 |
Table 5
Awareness regarding frequent vomiting can erode the enamel
|
|
Number |
Percentage |
|
Yes |
22 |
22 |
|
No |
78 |
78 |
Table 7
Aware of which trimester is the safe period for undergoing a surgical dental treatment during pregnancy
|
|
Number |
Percentage |
|
Yes |
22 |
22 |
|
No |
78 |
78 |
Table 8
Oral health practices among participants
Discussion
The aim of this survey was to assess the oral hygiene habits and awareness of oral health among pregnant women visiting the outpatient department of General Hospital, Muvattupuzha, Kerala. The survey also assessed the influence of educational qualification upon the oral hygiene during pregnancy on participants. The survey aimed to assess the relation of bleeding gums with different trimesters. All participants were having at least school level education.
In our study 35% of participants had complaints of bleeding gums while 21% had bad odor and 4% had gingival swelling. Our results were better than results obtained by Neha Gupta & Manisha Chhetry, in which they concluded that only 14% of participants in their study had reported of having bleeding gums. 6 This may be due to good oral health index, correct oral hygiene maintenance methods, gingival health can be maintained throughout pregnancy. 7
All 3 trimesters had reported bleeding gums and gingival swelling. This was constant with all the previous literatures.A huge number of participating members had a sound knowledge of oral hygiene habits. In our study, 91% of the participants used toothbrush to maintain oral hygiene. Dilip et al 8 reported in his study that 97% of participants who were educated used toothbrush. Pankaj et al. 9 reported a frequency of 98% and Sharda and Sharda et al 10 reported 94.4% in their respective studies. Our results were similar to results obtained by Kapoor et al. 11 where 90% used of toothbrush and toothpaste for maintaining oral hygiene. Though brushing is using toothbrush and toothpaste, the frequency of brushing still lags. Here, the number of people brushing their teeth twice daily was 14% only. These results are less than the results obtained by Jain et al. 12 in Jodhpur where 23% were brushing twice daily. 62% Kuwaitis, 13 67% Chinese, 14 and 90% of the US population 15 have been reported to brushing their teeth twice daily. According to our study, awareness was comparatively less in Keralite population than global standards though the literacy level is comparable with them. Hence awareness programs to improve oral hygiene habits are warranted in the study population.
A total of 15% participants were changing their brush monthly, whereas 34% were changing their brush every 3 months. This were better compared to the study by Jain et al. 12 where 60% respondents were changing their brush only when the brush became useless. Hence, the frequency of changing of tooth brush were better here. We also found that as the educational level increased, there is an increase in brushing frequency and frequency of changing the toothbrush.
It is well proved that regular dental procedures during pregnancy are fully safe and don’t adversely affect the pregnancy outcomes. 16 The safest period for dental treatment remains the second trimester where complex procedures such as minor surgeries can also be carried out. 17 But there is no need for deferring the dental treatments during pregnancy period as treatment after feotal organogenesis (2nd-3rd trimester) were also seen to be safe. 18 As per present study, only one quarter of participants (22%) were aware regarding safe trimester for undergoing a surgical dental treatment during pregnancy. Hence our study conclude that knowledge towards safest trimester for dental treatment was less in our study population.
Nausea and vomiting are common in early pregnancy (4th to 7th week after last menstrual cycle) in 50-90% of pregnant women. 19, 20 78% of our participants were not aware of that frequent vomiting can erode the enamel. Nausea and vomiting in pregnancy results in extensive erosion of the tooth surface which results in deterioration of their oral health status. 21 The elevated levels of gonadotropins in the first trimester, are reason for nausea and vomiting. Elevated amounts of progesterone, by a central-acting mechanism, decrease the rate of the gastric emptying. The gastric acids in the emesis, erode the enamel on the inner surface of the teeth, mostly the front teeth. 22 Erosion of the enamel can easily be controlled by advising the patients to rinse their mouths thoroughly after vomiting, with a solution that contains sodium bicarbonate. 23 Hormonal changes during pregnancy along with gastric acid exposure during recurrent morning sickness results in increased acidity in the oral cavity that can be a cause for eroding dental enamel.24, 25 Majority of participants were not aware of influence of vomiting during pregnancy on eroding enamel.
The most common barrier in seeking oral health care during pregnancy in our observation was due to not seeing oral health as priority. Considerable number of the females did not find visit to a dentist safe during pregnancy and avoided dental treatment unless it was an emergency. According to systematic study undertaken by Rocha et al, factors responsible as barriers are: physiological conditions, low importance towards oral health, negative stigma regarding dentistry, fear of/anxiety towards dental treatment, financial burdens, lack of employment, time constraints, social support, lack of knowledge regarding treatments, health professional’s barriers, relying on others advice, various beliefs and myths about the safety of dental treatment. 26 In our study, the main barrier we noted against seeking dental treatment was lack of seeing dental health as a priority.
69% of participants were aware of the fact that smoking or passive smoking, during pregnancy can lead to stillbirth, preterm delivery, low birth weight delivery, cleft lip and cleft palate, asthma, etc. But this was considerably less comparing with studies done by Motoc et al, according to which, 85% of all women were aware of bad effects of smoking on their and their babies health. 27 Maternal smoking during pregnancy (MSDP) is a big public health concern with clearly proved effects to both mother and newborn like low birth weight, altered cardiorespiratory responses, higher rates of poor cognitive and behavioral outcomes in children, including ADHD, conduct disorder, impaired learning and memory, and cognitive dysfunction. 28 It can also pose serious neurodevelopmental problems for the fetus, increased risk of intrauterine growth retardation, substance abuse, depression & hyperactivity. It is stated that both nicotine and Carbon monoxide decrease uterine blood flow, resulting in a state of hypoxia and malnutrition for the fetus. 29 Studies have results showing increased risk of stillbirth, both overall and for antepartum and intrapartum stillbirth. 30 In our study, majority of the participants were aware of the fact that smoking or passive smoking, during pregnancy
According to our study significant bleeding gums were observed in all trimesters. This was consistent with all the previous literature. Awareness regarding regular dental visits is less in our study participants as only 33% of them only visits dental clinics within 3 to 6 months. 37% had visited before 6 to 1 year. According to George et al, 31 30.5% reported to dentist in the last six months & according to Bogess et al 32 that 25% of participants visited a dentist during pregnancy. Awareness regarding dental visits are less if we compare with standard protocols.
The limitation of present study is its observational nature. Counseling and treatment if needed, must be provided to the participants along with creating awareness, which the study lacked. This study has the limitations of relying on self-reported data and can be subject to biases. It would have been better if assessment is made by a clinical examination of signs. This study was conducted among a small sample of pregnant women attending a single General hospital, Muvattupuzha.
Hence we can summarize from this study that, most pregnant women need more information about oral health and ways for prevention of occurrence of gingival and periodontal diseases. Our study subjects had reported more bleeding gums compared with other study populations. The main barrier we noted against seeking dental treatment was lack of seeing dental health as a priority. Majority were not aware of the effects of smoking or passive smoking, during pregnancy. Though literacy rate is high, the dental awareness was low and study population requires better awareness regarding safest trimester to carryout dental treatment and influence of vomiting during pregnancy on eroding enamel.
Conclusion
In spite of high literacy rate, majority of the pregnant women had minimum knowledge and information about oral health and its effect on the pregnancy. With this study, we can conclude that community level programs are required to educate pregnant women, regarding adverse pregnancy outcomes and its need for improving dental health. Dental care policies, must be developed to address these issues and policy makers should have an important role in addressing this. However study design with a randomized control trial will give more insight to this problem and it may be a further avenue for research.