Introduction
Oral thrush also known as oral candidiasis is an opportunistic infection of the oral cavity. Oral candidiasis is caused by yeast-like fungus known as candida. Symptoms of oral thrush can include white patches (plaques) in the mouth that can often be wiped off, leaving behind red areas that may bleed slightly, loss of taste or an unpleasant taste in the mouth, redness inside the mouth and throat, cracks at the corners of the mouth, a painful, burning sensation in the mouth. In some severe cases, the symptoms of oral thrush can make eating and drinking difficult. People with healthy immune systems, oral thrush rarely causes complications but in severe cases, it may spread to your esophagus.
Important species involved in oral thrush are C albicans (most common), C tropicalis, C glabrata, C pseudotropicalis, C guillierimondii, C krusei, C lusitaniae, C parapsilosis, and C stellatoidea. C albicans, C glabrata, and C tropicalis.1 Although oral thrush can affect anyone, but it is more likely to occur in babies and older adults because they have reduced immunity and in people with suppressed immune systems or certain health conditions or people who take certain medications.
Predisposing factors for oral thrush are 2
Table 0
Clinical classification of candidiasis 2
Table 0
|
Acute |
Chronic |
Other lesions |
|
Pseudomembranous |
Pseudo-membranous |
Angular cheilitis |
|
Erythematous |
Erythematous |
Denture-associated erythematous |
|
|
Hyperplastic |
Median rhomboid glossitis |
Management of oral thrush is oral hygiene and topical or systemic antifungals. Diagnosis is usually made on clinical grounds. Oral hygiene involves cleaning the teeth, buccal cavity, tongue, and dentures, if present, daily. Dentures should be cleaned and disinfected daily and left out overnight or for at least six hours daily. The dentures should be soaked in a denture cleaning solution such as chlorhexidine as this is more effective in eliminating candida than brushing.3 Predisposing factors should be treated or eliminated where feasible. Oral prophylaxis with antifungal agents reduces the incidence of oral candidiasis and fluconazole has been found to be more effective than topical polyenes. 4, 5
Case Presentation
A 40 years of age male patient came to dental clinic in the month of July, 2020 with chief complaints of white creamy patches over the tongue with burning sensations occasionally. On taking case history of patient he also revealed that he was suffering from the same for 6 months and had taken self-medications several times that include lignox gel and ibuprofen to relieve the symptoms of burning sensations, but these medicines gave no satisfactory relief to the patient and finally then he decided to visit the dental clinic on the advice of pharmacist. On taking medical and social history he told that previously he was a chronic smoker since the age of 20, but then he quit the smoking habit after being diagnosed with hypertension, hyperlipidemia and type 2 diabetes mellitus three years ago. Patient on detailed questioning related to his chief complaint revealed that he had a problem of bad breath, and whenever he tried to clean these patches with tongue cleaner & got these patches scrapped off, there were burning sensations & pain on taking hot, spicy and sour food items.
On examination & investigation intra-orally, it was found that there were white patchy lesions on the dorsal surface of tongue along with stains and calculus along with bad breath.
Random Blood Sugar- RBS level at that time in the clinic was 380 mg%, indicating uncontrolled diabetes in the patient.
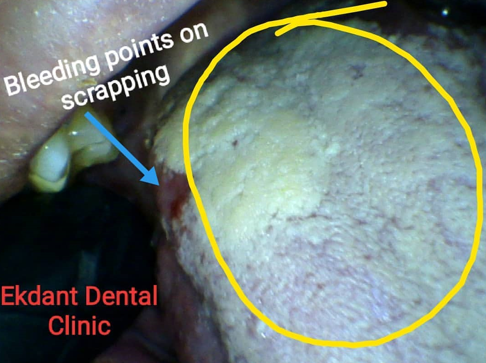
Clinical Visual findings- On intraoral examination, there were only white patches on the dorsal surface of the tongue. There was poor oral hygiene with the presence of calculus and stains in patient’s mouth (Figure 1).
Inspection- On inspection these white patches were like soft cotton present on tongue.
Physical Test- The lesions on scrapping gave small bleeding points that’s also suggestive of oral thrush (Figure 2). Unlike leukoplakia, the fungal patches can be scraped off. And it may result in bleeding at the site after removal and inflammation under the lesion and this inflammation, evident as redness and swelling suggestive of oral thrush.
On the basis of above clinical grounds, we reached to the provisional diagnosis of oral thrush due to the poor oral hygiene with a predisposing factor i.e. diabetes mellitus.
Treatment plan in this patient was
Patient education & two-way approach
Patient was instructed about the importance of maintenance of oral hygiene. Proper brushing and flossing techniques were demonstrated to the patient. The general physician was also called in dental office to motivate the patient for proper diet intake and lifestyle changes to control the predisposing factor in oral candidiasis i.e. hyperglycemia. Modification in the treatment plan was also done by the general physician to control the high blood sugar level.
Medications for thrush
The patient was prescribed with certain medications for the cure of this fungal infection.
Anti-fungal drugs ketoconazole tablet 150 mg OD x 7 dayTopical antifungal gel (clotrimazole) to be applied on tongue thrice a day x 14 days
Multivitamins Cobadex CZS twice a day for 1 month & Vitamin C tablets for 15 days.All these multivitamins either reduce the inflammation or strengthens the immune system or helpful in healing, and so these were prescribed to the patient.
Probiotics Patient was also advised to take probiotics sachets and as well as curd, yoghurt or buttermilk as these natural products are rich in lactobacillus that is good for thrush.
Analgesics
Analgesics were prescribed to reduce pain as well inflammation.
Oral prophylaxis
Oral prophylaxis was done four days later on 2nd visit after being the control of blood sugar level (Figure 3). The 0.2 % CHX mouthwashes and Septilin syrup were prescribed aa an adjunct to oral prophylaxis.
Results
From the above treatment plan patient’s oral health status began to improve just after 6 days, his blood sugar level was also controlled after changes in medication and life style changes. The burning sensation problem just resolved after 6 days of the treatment, and it took 22 days to completely disappear those fungal white patches. The patient was again instructed to keep his oral cavity clean.
The patient was recalled after 3 months for follow-up, on follow-up his tongue was free from candidiasis (Figure 4, Figure 5) and he never experienced any discomfort in 3 months. The patient was again instructed to maintain his oral hygiene.
Conclusion
Oral thrush can occur easily if oral hygiene is not maintained well and the chances of this further if a patient is already suffering from diseases like diabetes or HIV. The dentist must be well aware of oral manifestations of diabetes, thus enabling early identification of such infectious diseases, ensuring timely initiation of therapy. It is necessary to educate and motivate regarding the good oral hygiene as oral cavity is the gateway to body & poor oral hygiene can also lead to many systemic diseases.