Introduction
Mucous retention cysts or mucoceles are common oral benign lesions developed due to extravasation of the mucus from salivary glands where ranula is a comparatively rare form of mucocele found on floor of the mouth involving sublingual salivary gland. The name "ranula" is derived from the Latin word "rana" meaning "frog." The swelling of ranula resembles the transparent underbelly of a frog or air sacs. Normally the size o the lesion is greater than 2 cm and it appears as a painless, tense fluctuating dome-shaped vesicle, often with a blue hue.1, 2 This happens unilaterally mostly lateral to oral cavity floor and is usually seen in young adults with similar male and female prevalence.3 Research shows the prevalence approximately 0.2 cases per 1000 people, and account for 6% of all oral sialo-cysts. 4
In most cases the patho-physiology of ranula are not well understood and considered as unknown. The primary etiology for the development of ranula is partial obstruction of sublingual duct. This can contribute to the development of an epithelially-lined retention cyst, occurring in < 10% of all ranulas. The second most common factor is a wound that causes significant damage to the duct or deeper regions of the sublingual gland's body, leading to mucus extravasations and a pseudocyst formation. 5 The diagnosis, treatment planning and management of ranula is typically determined by a combination of history, clinical condition, histopathological appearance, and imaging studies.This paper presents management of large sized ranula in 8-year-old child with combination therapy of intra-lesional corticosteroid and micro-marsupialization.
Case Report
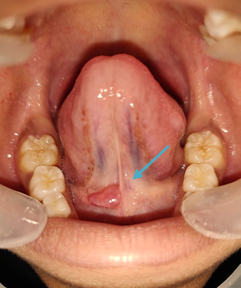
An 8 year old female patient reported to the department of Pedodontics and Preventive Dentistry with the chief complaint of painless swelling in the floor of the mouth with history of intermittent exaggeration and remission since past 4 months. General health of the patient was good with insignificant past dental, medical and family history. There was no history of trauma or injury related to oro-facial region. On intraoral examination, the lesion appeared as a translucent, dome-shaped bluish swelling in the right side of floor of mouth adjacent to the base of the tongue measuring approximately 1 cm in diameter. The lesion was smooth surfaced, fluctuating, soft in consistency and nontender on palpation. Reports of hematological and biochemical investigations were within normal limit. [Figure 1]
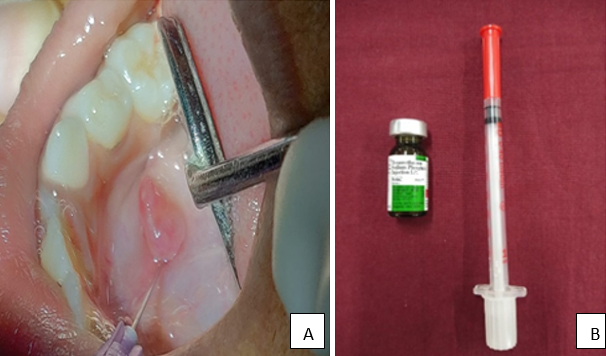
Based on history and clinical situation the patient was diagnosed with an oral ranula involving right sublingual gland. Evaluating the size of the lesion, age of the patient and patient’s parents requirement a combination therapy of intralesional injection followed by micro-marsupialization (if required) was planned. On the first appointment, patient and parent consents were taken after thorough discussion of treatment plan along with related benefit and risk. In the next appointment, a topical anaesthetic was applied to cover the entire lesion for approximately 3 minutes and aspiration of mucus was done with 3 ml syringe. Then 1ml of betamethasone (Decdan, 4 mg/1 ml) was slowly injected into the base of the lesion followed by periphery with an insulin syringe (0.3×8 mm size, 31gauge). The procedure was done gradually for being comfortable and painless. This procedure was repeated for 4 consecutive weeks (once in a week) until complete regression of the lesion. [Figure 2 ]
The patient was kept for 14 days observation and found recurrence of the lesion (5mm diameter in size). Next, the micro-marsupialization procedure was planned and discussed with the parent and appointment was fixed. Micro-marsupialization was performed on the next visit to drain the mucus and reduce the size of lesion. Under local anesthesia, a thick silk suture (3-0) was passed through the internal part of the lesion along its widest diameter followed by making a surgical knot and patient was called for follow up after 7 days. The 7th day healing was satisfactory without any post-surgical complications. Follow-up was done for 3 month, 6 months, patient was sound and showed no sign of recurrence. [Figure 3, Figure 4 ]
Figure 2
A) Mucous aspiration by 18-gauge needle and syringe B) 1ml of Betamethasone injection and 31 gauge insulin syringe.
Discussion
Mucoceles and ranulas located beneath the tongue areoften confused with other entities. The broad differential diagnosis can include hemangioma, lymphangioma, dermoid cyst, benign or malignant salivary gland neoplasm, lipoma, abscess, venous lake, fibroma or benign mesenchymal neoplasm. The diagnosis is often depends on clinical appearance of the mass along with a typical history of healing and recurrence similar to the present case. Diagnosis of the ranula is often supported with investigations like high-resolution ultrasound or sonography which is able to assess the lesion up to 90% of benign versus malignant tumours. 6 Ranula and mucocele can be demonstrated more clearly through the use of colour Doppler imaging. Computed tomography or magnetic resonance imagingare seldom necessary except in the case of a large or ‘plunging’ ranula, which may breech the mylohyoid muscle and present in the lateral aspect of the neck. 7 Detailed imaging can define the extent of the lesion and may be critical for the planning of surgery. Computed tomography and magnetic resonance imagingdo not differentiate between benign and malignant processes. Thus, a biopsy may be required for this purpose. The histological difference between ranula and mucocele is, the ranula is lined by granulation tissue, consisting of swelling and congested vasculation whereas, mucocele consist of ductal epithelium. 8
Managing a ranula depends on a variety of variables but primarily on its size and location. In the process of removing stones from the hilum of the submandibular gland, a technique has been developed which requires that the sublingual gland be mobilized and rotated laterally on the floor of the mouth.9 Small, well-located ranulas respond to local excision much the same as mucoceles on the lower lip. The surgical removal of ranula along with the associated sublingual gland is the most predictable method of getting rid of the lesion. Although, it is not necessarily an easy operation, but can be considered more successful if carried out in a clean, bloodless environment. Unfortunately, the morbidity of the removal of sublingual gland is relatively high.
Also, the chance of injury to the Wharton duct (2%), bleeding (1% to 2%), infection (1% to 2%) or lingual nerve paraesthesia (2% to 12%) may increases. A number of more progressive approaches that are consistent with office practices have been suggested, including laser de-roofing, 10 cryotherapy, suture ligation, and marsupialization variation. 11
Micromarsupialization has been shown to be a simple, fairly non-invasive, painless, efficient and low recurrence technique used by Amaral et al.(2012) and Sagari et al(2012) to treat oral ranulas and selected mucoceles, in which all cases showed complete healing within 30 days of the procedure. Nonetheless, these surgical procedures have many drawbacks, such as trauma, discomfort, lip disfigurement, damage to adjacent vital structures, and ducts that contribute to the creation of satellite lesions, and can also be costly for the patient. 12 Thus, a non-surgical treatment regimen with extremely active corticosteroids (betamethasone) has been introduced. Intracystic injection therapy with OK-432 (a lyophilized mixture of low virulence strain of streptococcus pyogenes incubated with benzyl penicillin) has been reported to be relatively safe and can be used as a surgical substitute for ranula therapy. 13 Ranula can be treated with a silk suture placed in the cyst dome as a process of micro-marsupialization. Pandit and Park(2002) suggested that successful pediatric oral cavity management may involve observation of spontaneous resolution for 5 months. Unless the lesion doesn't regularly heal or recur, surgical therapy is prescribed. Hence the decision to perform combination therapy of intralesional corticosteroid and micro-marsupialization was taken as per the clinical situation.14, 15
Conclusion
Surgical management of oral lesion is often difficult in pediatric patients under local anaesthesia. Therefore, the combination therapy of intralesional corticosteroid and micro-marsupialization can be a treatment option instead of direct surgical excision in children. More cases with long-term observations are needed to assess the success of this therapy in children.