Introduction
One of the commonly used polymers in dental field is poly-methyl methacrylate (PMMA), which uses either heat polymerized or self-polymerized acrylic resin. The popularity of acrylic resin is related mainly to its ease in manipulation, ease in finishing and polishing, as well as it needs inexpensive equipment.1 Furthermore, the acrylic resin has good stability in the oral conditions and has high aesthetic quality. However, it has limitations including low thermal conductivity, a high thermal expansion coefficient, a low elastic coefficient, low impact strength, and a low resistance to fatigue. 2 Poly-methyl methacrylate resin denture base material has poor surface properties and weak mechanical properties including impact and flexural strengths. The fracture resistance of Poly-methyl methacrylate is not satisfactory. According to a survey, two-third of dentures had broken within three years of their provision. 3 Therefore, resins should be reinforced using different materials to enhance their properties.
Recently, nanotechnology invaded the dental field and initiated investigative research projects to explore the possible applications and expected benefits within dentistry. Nanoparticles have extremely high surface area to volume ratios, and can alter the mobility of polymer chains near their interfaces. So, even a small addition of nanoparticles has the potential to drastically transform the properties of the host polymer. 4 Various nanoparticles are incorporated into the polymer matrix for nanocomposite applications. Among them, nanocomposite with nanoscale Titanium dioxide has gained great interests to scientists.
Titanium dioxide nanoparticle has proved to have antimicrobial properties. Moreover, it is a cheap biocompatible material, chemically stable, free of toxicity, resistant to corrosion with high strength, and high refractive index. Even the slight addition of titanium dioxide nanoparticle reinforcing agent to a polymeric material affects the electrical, optical, chemical, and physical properties of the resulting hybrid material. 5 Flexural fatigue and impact fracture have been implicated as a mechanism of denture fracture. Therefore, the transverse strength of the denture base materials can be an important indicator of their performance.
This study evaluates the effect of Titanium dioxide nanoparticle on tensile and impact strength in normal and veined type of acrylic denture base materials.
Materials and Methods
Armamentarium
The following materials, instruments, and equipment were used in this study.
Materials
Heat cure acrylic denture base resin, Pink (DPI Heat Cure, the Bombay burmah trading corporation ltd, India)
Heat cure acrylic denture base resin, Veined (DPI Heat Cure, the Bombay burmah trading corporation ltd, India)
Titanium dioxide nanopowder (Nanoshel, Purity – 99.9%, Average particle size – 10-25 nm)
Cold mold seal (DPI, The Bombay Burmah Trading Corporation Ltd., Mumbai)
Cellophane sheet
Modelling wax
Dental stone
Water cooled silicone carbide paper
Study Setting
Department of Prosthodontics and Crown And Bridge, Government Dental College, Trivandrum.
College of Pharmaceutical Sciences, Government Medical College, Thiruvananthapuram.
CIPET: Institute of Plastics Technology, Kochi.
Sree Chitra Tirunal Institute for Medical Sciences & Technology (SCTIMST), Poojapura, Thiruvananthapuram.
The study was conducted in the Department of Prosthodontics, Government Dental College, Thiruvananthapuram. The mixing of polymethyl methacrylate (PMMA) with titanium dioxide nanoparticle was done in College of Pharmaceutical Sciences, Government Medical College, Thiruvananthapuram. Fabrications of moulds and testing of tensile strength were done in Sree Chitra Tirunal Institute for Medical Sciences and Technology, Poojapura, Thiruvananthapuram. Testing of impact strength was done at CIPET Center for Biopolymer Science and Technology, Kochi.
Study Specimen
1. For tensile strength :
Rectangular specimen (60mm x 10mm x 2mm).
Group A1 – Heat activated acrylic resin.
Group A2 – Heat activated acrylic resin incorporated with 1 wt. % titanium dioxide nanoparticles.
Group B1 – Heat activated veined acrylic resin.
Group B2 – Heat activated veined acrylic resin incorporated with 1 wt. % titanium dioxide nanoparticles.
2. For impact strength
Rectangular specimen (80mm x 4mm x 10mm).
Group C1 – Heat activated acrylic resin.
Group C2 – Heat activated acrylic resin incorporated with 1 wt.% titanium dioxide nanoparticles.
Group D1 – Heat activated veined acrylic resin.
Group D2 – Heat activated veined acrylic resin incorporated with 1 wt.% titanium dioxide nanoparticles.
Sample Size
Sample size was calculated independently for tensile and impact strength testing by taking the necessary values from previous studies. 4, 6 The type I error was set to 5% and type II error was set to be 20% making the power of the study 80%. After doing the calculations the sample size was taken as 10 for each group, there are 8 groups and hence total sample size was 80.
Procedure
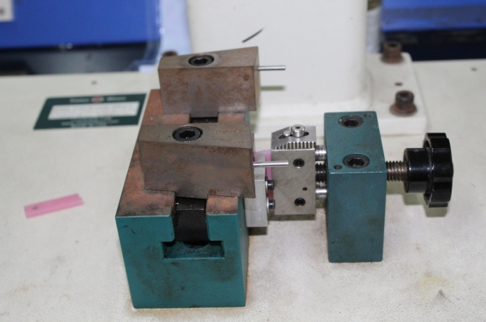
Fabrication of stainless steel mould
To make the specimens, uniform stainless steel moulds were made (Figure 1). Two stainless steel moulds, one of dimension 60mm x 10 mm x 2 mm (rectangular shaped) for tenilse strength and another of dimension 80mm x 4mm x 10mm (rectangular shaped) for impact strength testing specimen fabrication.
Modifying polymethyl methacrylate powder by incorporation of titanium dioxide nanoparticles particles
The required amount of the titanium dioxide nanoparticles was one weight percentage (1wt%). The appropriate amount of titanium dioxide particles and PMMA powder were weighed using a digital weighing balance and mixed together using mortar and pestle. To ensure the uniform distribution of titanium dioxide nanoparticles geometric dilution method was employed. Where in larger mass material is added in small portions into the less mass substance. This process is repeated until the entire larger mass is added to the smaller one. The measured quantities were:
Fabrication of heat activated acrylic resin specimens
The stainless steel mould was used to make the wax patterns for the fabrication of the acrylic resin specimens (Figure 2). After dewaxing and processing all specimens were trimmed, smoothened, finished and polished using water-cooled silicone carbide papers. Dimensions of specimens were measured using a digital Vernier caliper with measuring accuracy of ±0.1 mm. Specimens were then stored in the water bath at 370C till the tests were conducted. They were removed from water one hour prior to testing to obtain a dry specimen. Total 80 specimens were fabricated.
Testing for tensile strength
Tensile strength was tested using the universal testing machine (INSTRON)(Figure 3). (Sree Chitra Tirunal Institute of Medical Science and Technology, Thiruvananthapuram). The rectangular specimens were inserted in relative jigs on a universal tensile testing machine and jigs were tightened (Figure 4). The apparatus exerted increasing tensile force at a crosshead speed of 5 mm/minute until the specimen fractured, and the load at the time of fracture was recorded as it appears in the computer monitor connected to the apparatus. The same procedure was repeated for all 40 specimens, and readings were expressed in Mega Pascal(MPa) (Table 2).
Tensile strength in MPa was calculated using the following formula.
S=
Where T.S = Tensile strength, MPa
F = Load at the time of fracture, N
A = Cross-sectional surface area, mm2
Table 2
Tensile strength
Testing for impact strength
The IZOD impact tester was used to evaluate the impact strength of each specimen (Figure 5,6). IZOD is a pendulum impact machine consisting of a base, a pendulum and a striker rod. The 80mm x 4mm x 10mm rectangular specimens will be inserted in the anvil to receive the blow of moving mass. For plastic type material like the acrylics the pendulum apparatus imparting the load is half disc shape. Initially the machine was caliberated to reduce the error, the test specimen is held tightly in the anvil, the pendulum is then released from its latch. Pendulum swings down gaining energy from gravitational force and the height from which it is released. It hits on to the specimen and the specimen breaks and the pendulum swings to the other side.
The impact strength is calculated as follows
The mass of the hammer mass (m) is raised to a height (a)
Initial energy = mga
g = gravitational force
final energy = mgb
b = hammer raised to height after impact fracture of specimen
so energy absorbed during impact = mg(a-b). It is expressed in Kj/m2 (Table 3)
Table 3
Impact strength
Results
Data were analyzed using computer software, Statistical Package for Social Sciences (SPSS) version 25. Data were expressed in its mean and standard deviation. Since the units are continuous variable, the analysis will be performed by t-test to compare the tensile and impact strength of conventional acrylic and veined acrylic modified with titanium dioxide nanoparticle incorporation and also to compare the conventional and veined acrylic followed by Bonferroni’s correction to control the p value. For all statistical evaluations, a probability value, <0.05 is considered significant.
The maximum mean tensile strength was seen for group A2 and the least was seen for group B1. (Table 4).
Table 4
Tensile strength (Mpa)
| Group | Mean | Standard Deviation | 95% Confidence Interval Of Mean |
| A1 | 53.21 | 10.36 | 45.80 – 60.63 |
| A2 | 56.87 | 3.96 | 54.03 – 59.70 |
| B1 | 44.48 | 3.31 | 42.11 – 46.85 |
| B2 | 53.16 | 4.62 | 49.85 – 56.41 |
The maximum mean impact strength was seen for Group C2 and least was for group D2 (Table 5. The statistical significance was evaluated with t test followed by Bonferroni’s correction to control the p value.
Table 5
Impact strength (KJ/m2)
| Group | Mean | Standard Deviation | 95% Confidence Interval Of Mean |
| C1 | 8.72 | 0.78 | 8.16 – 9.28 |
| C2 | 10.10 | 0.40 | 9.81 – 10.39 |
| D1 | 9.23 | 0.34 | 8.98 – 9.47 |
| D2 | 7.01 | 0.66 | 6.54 – 7.48 |
Table 6
Comparison between A1 and A2
| Comparison groups | Mean | Standard deviation | Test used with value | P value and significance |
| A1 | 53.21 | 10.36 | t = 1.04 | 0.311 |
| A2 | 56.87 | 3.96 |
The comparison between group A1 and A2 showed the p value to be 0.311 making it statistically insignificant (Table 6). This indicates that there is no significant change to the conventional acrylic and the one modified with titanium dioxide.
Table 7
Comparison between B1 and B2
| Comparison group | Mean | Standard deviation | Test used with value | P value and significance |
| B1 | 44.48 | 3.31 | t = 4.83 | < 0.0001, HS |
| B2 | 53.16 | 4.62 |
The comparison between group B1 and B2 showed the p value to be < 0.0001 making it Highly significant (HS) (Table 7). That is the veined acrylic modified with 1wt% TiO2 showed increased tensile strength compared to the unmodified veined acrylic.
Table 8
Comparison between A1 and B1
| Comparison groups | Mean | Standard deviation | Test used with value | P value and significance |
| A1 | 53.21 | 10.36 | t = 2.54 | 0.021, sig |
| B1 | 44.48 | 3.31 |
The comparison between group A1 and B1 showed the p value to be 0.021 making it statistically significant (Table 8 ) indicating the conventional one showed increased tensile strength compared to the veined acrylic.
Table 9
Comparison between A2 and B2
| Comparison groups | Mean | Standard deviation | Test used with value | P value and significance |
| A2 | 56.87 | 3.96 | t = 1.93 | 0.070 |
| B2 | 53.16 | 4.62 |
The comparison between group A2 and B2 showed the p value to be 0.070 making it statistically insignificant (Table 9). There is no significant change between the 1wt% TiO2 modified conventional acrylic and the veined acrylic modified with 1wt% TiO2.
Table 10
Comparison between C1 and C2
| Comparison group | Mean | Standard deviation | Test used with value | P value and significance |
| C1 | 8.72 | 0.78 | t = 4.95 | < 0.0001 |
| C2 | 10.10 | 0.40 |
The comparison between group C1 and C2 showed the p value to be <0.0001 making it highly significant (HS) (Table 10). That is there is significant difference in impact strength between conventional acrylic and the one modified with 1wt% titanium dioxide which shows an improvement in impact strength.
Table 11
Comparison between D1 and D2
| Comparison groups | Mean | Standard deviation | Test used with value | P value and significance |
| D1 | 8.72 | 0.78 | t = 4.95 | < 0.0001 |
| D2 | 10.10 | 0.40 |
The comparison between group D1 and D2 showed the p value to be <0.0001 making it highly significant (Table 11). There is decrease in impact strength of the modified veined acrylic compared to the normal veined one.
Table 12
Comparison between C1 and D1
| Comparison groups | Mean | Standard deviation | Test used with value | P value and significance |
| C1 | 8.72 | 0.78 | t = 1.87 | 0.086 |
| D1 | 9.23 | 0.34 |
The comparison between group C1 and D1 showed the p value to be 0.086 making it statistically insignificant (Table 12 ). This indicates that there is no significant difference in impact strength between conventional acrylic and the one veined acrylic in impact strength.
Table 13
Comparison between C2 and D2
| Comparison groups | Mean | Standard deviation | Test used with value | P value and significance |
| C2 | 10.10 | 0.40 | t = 12.60 | < 0.0001 |
| D2 | 7.01 | 0.66 |
The comparison between group C2 and D2 showed the p value to be <0.0001 making it highly significant (Table 13). There is higher impact strength of the modified conventional acrylic compared to the modified veined one.
Discussion
In many cases a conventional complete denture is still the preferred treatment of choice considering medical and financial reasons. 7 An ideal denture base material should have adequate mechanical and physical properties, besides biocompatibility and aesthetics. Poly methyl methacrylate (PMMA) is used to fabricate denture bases due to its various advantages, including low cost, biocompatibility, ease of processing, stability in the oral environment, and acceptable aesthetics. 8
However, it cannot be considered as an ideal material due to its inferior physical and mechanical properties. The major drawback of PMMA is its inadequate mechanical and physical properties such as low flexural strength (FS), impact strength (IS) and surface hardness that leads to reduced clinical performance of the denture. This ultimately leads to reduced clinical life of the prostheses, and hence increases the patient’s dental visits and the cost factor. 9
Dentures are known to undergo various failures such as fractures, debonding of the teeth, and other types of failures in complete or partial dentures. According to a survey conducted by Darbar et al 10 on the causes of repairs involving complete and partial dentures, it was reported that 29% of all repairs to dentures were associated with midline fractures of complete dentures and 68% of acrylic resin denture break within a few years after fabrication caused primarily by impact failure when the denture is accidentally dropped on a hard surface or by fatigue failure when the denture base deforms repeatedly under occlusal force. 9 In maxillary dentures, most fractures are caused by a combination of fatigue and impact, whereas in mandibular dentures, 80% of fractures are caused by impact alone. Maximum fracture was seen in the denture age group of two to four year post-delivery followed by zero to two years. 11 According to Naik AV 11 accidental dropping of the denture while cleaning, insertion and removal (53%) was the most common cause for lower denture fracture followed by poor retention and fit (22%) whereas poor fit was the most significant factor for upper denture fracture (43%) followed by accidental dropping of the denture (25%) .
Many techniques have been used for improving mechanical properties such as chemical correction of polymeric structure by additives like polyethylene glycol di-methacrylate. The other useful method is to reinforce acrylic base composite by materials like fibers and particles. 4, 12, 13 One approach is to increase its mechanical properties by the incorporation of a rubber phase in the bead polymer but this modification process is quite expensive. Another approach used is by reinforcement of the denture base polymer with various reinforcement materials such as metal oxides, polyaramid fibers, stainless steel wires, and mica. 9
The principle behind the usage of nanoparticles is that alteration of filler size is considered responsible for the performance of the material (PMMA) in aspects of both polishability and fracture resistance. 14 Various nanoparticles (NP) have been added to different dental materials like titanium dioxide (TiO2), silico dioxide (SiO2), zinc oxide (ZnO), silver (Ag), copper oxide (CuO) etc. in order to induce antimicrobial property. Amongst these, TiO2 has received recent attention because of its prominent catalytic effect, white color, low toxicity, high stability, efficiency, availability and low cost. 15 The anti microbial and anti fungal properties of the titanium modified acrylics has been proven.16, 17, 18 According to study by Totu 18 the modified acrylic was evaluated for anti microbial properties and found that 0.4, 1% and 2.5% TiO2 inhibited candida growth. The results of study of Masashi tsuji 19 demonstrated that denture base coated with TiO2 does not cause irritation or sensitization of oral mucosa, skin or intra-cutaneous tissue and hence has good biocompatibility.
In this study incorporation of titanium dioxide nanoparticles into two different types of acrylic denture base resins (heat cure conventional acrylic and heat cure veined acrylic) was done to evaluate the tensile strength and impact strength. Geometric dilution method of powder mixing was used to get a uniform mix. 1wt% TiO2 was employed based on previous studies. According to Muhammet karci 20 to evaluate flexural strength of different denture base resins reinforced with different nanoparticles aluminium oxide (Al2O3) SiO2 and TiO2. The flexural strength values decreased with increased addition of nanoparticles and the study concluded that 1 wt% of fillers can be considered as the ideal filler ratio. According to M. A. Ahmed et al4 addition of 1% TiO2 Nanoparticles(NP) to conventional resin improves impact strength, 21, 22, 23 on the other hand, higher concentrations (5% TiO2) will lead to impact strength deterioration of the resin material.
Tensile strength was tested using universal testing machine. It was found that tensile strength difference was not statistically significant for the 1wt% modified conventional heat cure acrylic resin compared to the conventional acrylic resin. But the maximum tensile strength was observed for the 1 wt% TiO2 modified conventional acrylic. While the difference in the tensile strength was highly significant for 1 wt% TiO2 modified veined acrylic compared to normal veined one. The results of veined acrylics are in accordance with the study of Shirkavand and Moslehifard24 where in there was a significant increase in tensile strength values in TiO2 nanoparticles-acrylic resin containing 1wt% TiO2. The additional TiO2 nanoparticles act as impurities and the tensile strength decreases as a result of the extra additives. The study by Ghahremani et al 6 showed addition of 1wt% TiO2 particles to acrylic resin significantly increased its tensile strength. Acosta-Torres et al 24 stated that metal oxides are suitable for addition to acrylic polymers to enhance their mechanical properties and showed that titanium dioxide nanoparticles improved the mechanical properties of resins. The current study also shows the same results as shown by the above studies.
In the current study impact strength determination were tested using IZOD impact tester. It was found that maximum impact strength was noted to the 1wt% TiO2 nanoparticles modified conventional heat cure acrylic and the least was for the 1wt% TiO2 nanoparticles modified veined heat cure acrylic. There is highly significant difference in impact strength between conventional acrylic and the modified conventional acrylic which proved to be better.
Ghahremani et al 25 evaluated the tensile strength and impact strength of 1wt % TiO2 NP modified SR Triplex Hot, heat cure acrylic. The study stated that both tensile and impact strength increased with addition of the titanium dioxide nanoparticles. The results of the current research are in accordance with this study. Unlike the present study Neset volkan et al, 25 evaluated the effect of various metal oxides on impact strength, fracture toughness, water sorption and solubility of heat cured acrylic resin. The oxide powders used were aluminium oxide (Al2O3), titanium oxide and zirconium oxide. The results showed that the addition of metal oxides improved impact strength and fracture toughness while there was decrease in the water sorption and solubility but no study has been conducted regarding the tensile strength of the material. In study conducted by Tiba and Hanan 26 modified zirconia oxide – titanium oxide nanoparticles on certain physical and mechanical properties of heat polymerized acrylic resin was evaluated. Results showed a significant increase in impact strength like in present study but no significant change in thermal conductivity was observed.
Ahmed et al 4 compared flexural strength, impact strength, and hardness of Conventional heat cure acrylic resin and high impact heat cure acrylic resin modified with 1.0%, 5.0% TiO2 nanoparticles. Impact strength was found to be enhanced Increased only for conventional acrylic resin modified by 1 percentage. In another study Aziz 27 evaluated the impact strength, color stability, and thermal conductivity of High impact heat cure acrylic resin (Vertex-Dental, Netherlands) reinforced with addition of 3.0% of TiO2 NP. Impact strength increased and color stability also improved but there was no effect on the thermal conductivity.
In the present study the 1wt% TiO2 modified veined acrylic had less impact strength compared to the conventional veined acrylic and also the least among all. The increase in filler content (both veined fibers and the nanoparticles) causes these particles to agglomerate. The agglomerated compounds can act as stress concentrating centers in the matrix and adversely affect the mechanical properties of the polymerized material. The agglomeration of TiO2 probably gives rise to some micro-pores and micro-crack as structural defects. 24 Any attempt to add filler particles after reaching saturation of matrix leads to interruption in the matrix continuity and thus leading to a decrease in the strength of reinforced specimens. 4
Titanium dioxide nanoparticles incorporation in the present study showed an increase in the impact strength of the conventional acrylic while the incorporation in the veined acrylic decreased impact strength. There is also an increase in the tensile strength for the modified veined acrylic while there is no considerable change in the conventional modified acrylic. The improvement in mechanical properties of conventional heat cure acrylic have been achieved with untreated titanium nanoparticles without additional procedure of silanization. Hence denture fabrication by this method will not be time consuming, and more economic as well.
The limitation of this study was that only a single optimum weight percentage was used as the increase or decrease in the weight percentage is found to be statistically insignificant. The present study evaluated only the changes in two properties like impact strength and tensile strength. The change in other properties of the material in these concentrations of titanium nanoparticles addition should be investigated. Since the present study was an in-vitro study, the results could not be applied to any clinical situation whatsoever.
Conclusion
The present study was conducted to evaluate the effect of incorporation of one weight percentage titanium dioxide nanoparticles to two different types of poly methyl methacrylate in terms of two properties tensile strength and impact strength. The results showed that the addition of titanium dioxide nanoparticles significantly increased the impact strength of the conventional heat activated acrylic denture base resin while there was no significant change with tensile strength, whereas incorporation of titanium dioxide nanoparticles significantly decreased the impact strength of veined acrylic denture base resin. The current study shows that the titanium dioxide nanoparticles should not be used in free will in all types of acrylics to reinforce them. In spite of the limitation of the material in aspect of impact strength of veined acrylic the titanium dioxide nanoparticles can be recommended to be used in the reinforcement of dentures with conventional heat cure acrylic.